Adolescent Idiopathic Scoliosis: Towards Improved Surgical Results Thanks to AI
Adolescent idiopathic scoliosis (AIS) is characterized by a structural curvature of the spine, typically seen during the adolescent growth spurt. It is the most common form of scoliosis, affecting approximately 1 to 4% of adolescents, with a higher prevalence in young girls than in boys. If left untreated, scoliosis can lead to changes in spinal mechanisms, degenerative changes, and various health problems, including pain, loss of spinal mobility, and reduced quality of life.
Posterior spinal fusion (PVF) constitutes 90% of scoliosis-related surgical procedures, with approximately 38,000 operations performed each year in the United States. The decision to intervene on a patient with idiopathic scoliosis depends on many factors: maturity of the patient, characteristics of the curvature, location and possibility of progression of the malformation. As most individuals with AIS experience worsening during periods of growth, the primary goal of intervention is to limit or stop this progression. Therefore, improving the patient’s quality of life is essential.
As part of regular scoliosis care, patients undergo serial x-ray examinations and detailed measurements to plan surgery, evaluate corrections made, and follow-up (i.e., rehabilitation) over time. The development of the Scoliosis Research Society (SRS) Patient Quality of Life Questionnaire allowed orthopedists to measure subjective outcomes reported by patients before and after corrective surgery. The SRS-22R stands out as one of the most used tools to assess the quality of life of patients with AIS, taking into account aspects such as function, mental health, pain, satisfaction and image of oneself. However, preoperative radiographic parameters, often used during surgical planning, have not yet shown a correlation with postoperative subjective outcomes. It is therefore essential to clarify this relationship to help surgeons better define expectations for patients and their families.
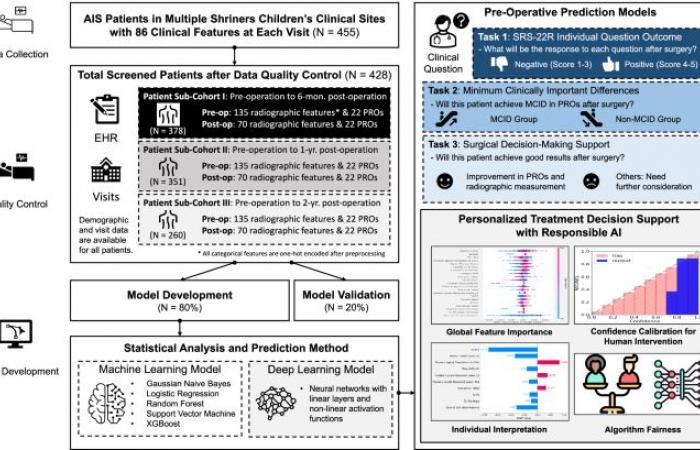
To address this issue, we developed an AI-assisted surgical planning support and advisory system to predict rehabilitation outcomes of AIS patients after FVP, based on a multicenter pediatric cohort. Our studies were conducted on a group of 455 young patients who underwent spinal fusion at two Shriners Children’s hospitals since 2010. This cohort is unique, due to the rarity of cases of severe AIS (less than 0.1% in the United States). United). We sought to predict three key outcomes that would facilitate surgical planning and shared decision-making: postoperative response to each SRS-22R question, achievement of the minimal clinically important difference, and improvement in objective radiographic measures as well as subjective self-assessment of patients. Additionally, we conducted explainability analyzes and statistical analyzes to quantify the impact of preoperative radiographic parameters and self-reported outcomes to clinically validate our approach. We also incorporated responsible AI considerations by calibrating model confidence to intervene at the right time and reducing gender bias.
Electronic health record, PRO patient-reported outcome indicator.
In summary, our contributions revolve around three axes: first, we carried out an exhaustive analysis on a multicenter cohort of AIS patients with post-operative follow-ups of 6 months to 2 years, in order to develop a predictive model of post-operative results; then, we created a surgical planning support system aimed at predicting patients’ surgical outcomes based on subjective improvements and objective radiographic measurements for a personalized surgical plan; Finally, we have integrated explainable and responsible AI considerations into our approach to ensure fairness and better understand the clinical outcomes obtained.
Takeaways
- AIS affects 1 to 4% of adolescents, with a higher incidence among young girls.
- FVP is the primary form of surgical treatment for scoliosis.
- The SRS-22R questionnaire is widely used to assess patient quality of life outcomes.
- Advanced AI technologies are leveraged to predict post-operative outcomes and facilitate personalized decision-making.
- Current work shows that research is focusing more on adult patients than adolescents, highlighting a potentially under-researched area.
This innovative development in the field of scoliosis could mark a major advance in pediatric care. As technology and AI continue to transform healthcare, it is critical to ask how these advances can be extended to other areas of medicine and what lessons can be learned to further improve the quality of care provided to the youngest patients.
- Source image(s) : www.nature.com
- Source : https://www.nature.com/articles/s43856-024-00726-1
Our editors use AI to help them deliver fresh items from trusted sources to our users. If you find any image or content that is inappropriate, please contact us via DMCA form and we will promptly remove it. / Our editors use AI to help them offer our readers fresh articles from reliable sources. If you find an image or content inappropriate, please contact us via the DMCA form and we’ll remove it promptly.





