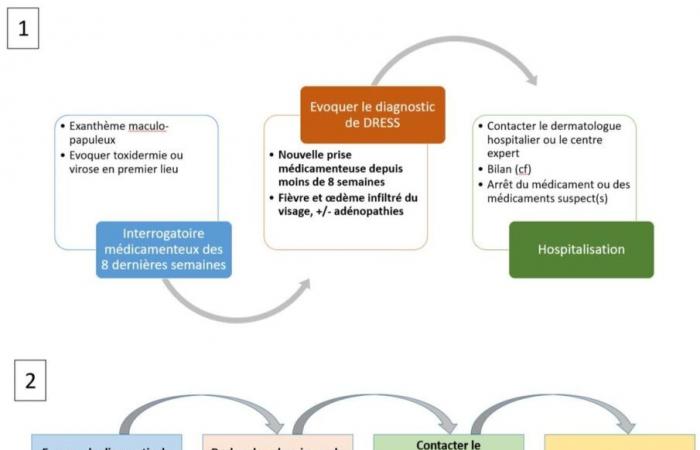
If DREES is suspected, the general practitioner must:
- immediately stop the drug(s) suspected of being responsible;
- refer the patient to a local emergency service which will complete the assessment, or even contact the SAMU if there are serious hemodynamic, respiratory and/or neurological signs;
- and/or directly contact a dermatologist or a hospital dermato-allergist in connection with a expert center for serious drug addiction (to be found on the website: https://toxibul.fr/).
The general practitioner can initiate, depending on the extent of the rash and the patient’s discomfort, a very strong local corticosteroid therapy (clobetasol) and emollients, but should avoidunless there is an obvious manifestation of serious DRESS and unless specialized advice is given, any general corticosteroid therapy (risk of ruining the table and rebounding of the DRESS when stopped).
In the expert center, the diagnosis is confirmed and the severity of the DRESS is established. The assessment is completed and a skin biopsy is performed. Replication of the HHV6, EBV and CMV viruses is sought by blood PCR (even if their role is debated). There is no need to urgently search for these viral replications in the citybecause they do not influence the initial treatment of DRESS and are not reimbursed. There is no point in carrying out serologies.
The treatment of DRESS is based on corticosteroid therapy, local or general depending on the severity, which is gradually stopped over a period of 3 to 6 months. Stopping too quickly and abruptly exposes you to a relapse or rebound of DRESS, sometimes with serious visceral damage (myocarditis).
After the acute phase, monitoring remains tight until complete normalization of clinical and biological parameters. Autoimmune sequelae, including thyroiditis and diabetes, may occur weeks or months after apparently complete recovery from DRESS.
At a distance from the acute phase, allergological skin tests carried out by a dermato-allergist expert are useful to confirm, if they are positive, the drug attributability. However, negative tests do not exclude liability for a drug. The molecules held responsible, and those of the same chemical class, are formally contraindicated for life. The patient must inform the general practitioner of the allergy card given to them. The hospital doctor is responsible for the pharmacovigilance declaration.
Attending physicians must be made aware of the possibility of autoimmune sequelae, to be screened for in the year following the acute phase. Finally, it is important to advise the patient to consult urgently in the event of chest pain and dyspnea even after the acute phase of DRESS, so as not to overlook myocarditis.