In France, 5,634 organ transplants were carried out in 2023, or 2.5% more than the previous year. But although activity may be growing, the provision of care remains insufficient: nearly 11,500 patients are on the waiting list and 823 have died because they did not obtain a transplant in time. This shortage of organs is not specific to France: according to the World Observatory of Donations and Transplantation, the 150,000 transplants carried out worldwide only cover 10% of needs.
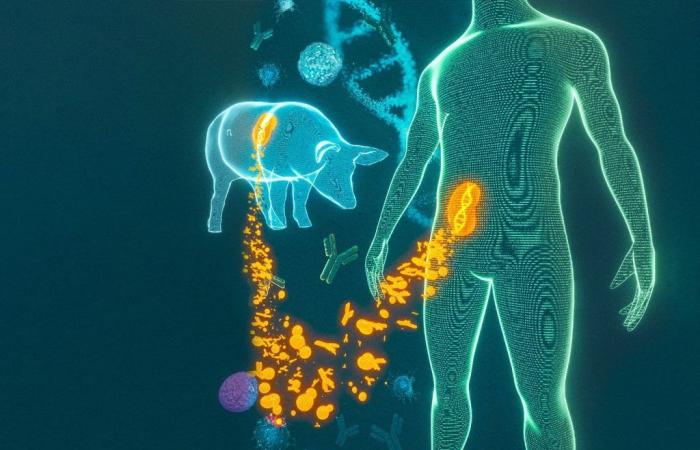
Hence the hope aroused by research on xenograft or xenotransplantation, an operation which consists of replacing a deficient organ in humans with an animal organ. A field that has been progressing at high speed for several years. “This progress is mainly due to the emergence of biotechnologies like that of the Crispr-Cas9 molecular scissors which make it possible to manipulate living things”recalls Professor Olivier Bastien, former director of sampling at the Biomedicine Agency. And at the same time tackle the major problem that xenotransplantation has long faced: that of the incompatibility between an organ from another species and the human immune system, which means that the recipient’s antibodies will destroy the graft in the minutes following transplantation.
“Humanized” pigs
To overcome the obstacle, scientists had the idea of “making” transgenic pigs in which we will inhibit certain genes harmful to the transplant and insert human genes to make them more compatible. “Pigs that are, in a way, humanized, whose breeding, through cloning, provides an almost unlimited source of organs for humans”underlines Olivier Bastien.
And for several years, the “firsts” have been coming one after the other. On January 7, 2022, David Bennett, 57, became the first living patient transplanted with a transgenic pig heart by a team from the University of Maryland. On March 16, 2024, Richard Slayman, 62, entered the annals of history as the first patient to receive a genetically modified pig kidney at the Massachusetts General Hospital in Boston.
In both cases, the patients died within two months following the intervention, which does not prevent specialists from describing these clinical trials as “major advances”. Rightly so, since they made it possible to establish that the risk of so-called “hyperacute” rejection could be overcome. But the enthusiasm of researchers cannot obscure the ethical questions, sometimes dizzying, that these technical feats raise.
The first concerns the interests of patients and the famous benefit-risk balance which governs medical conduct. Given the mixed results obtained, should these trials be continued and with which patients? For the moment, the experiments carried out in the United States have been on people who are brain dead or for whom xenograft was the last hope.
“But if we only perform xenografts on patients at the end of life, we will not be able to assess their real benefit. When it comes to pioneering work, you have to know how to take risks, while surrounding yourself with precautions to control them as best as possible,” estimates nephrologist Valentin Goutaudier, researcher at the Transplant Institute of Paris Cité University (Pitor).
Threats to the gift economy
One risk worries more than others: that of a possible transmission of a pathogen from animals to humans. “In the 1990s, mad cow disease brought all programs to a complete halt”recalls Olivier Bastien. The world then discovered the danger of zoonoses. He has since learned to adapt.
“The pigs that provide the organs are genetically modified to deactivate the viruses they ancestrally carry and are raised in a 100% sterile environment,” he continues. And transplant patients are closely monitored. “At the slightest alert, the programs will be stopped”supports Valentin Goutaudier.
Added to these technical challenges is an economic issue: will xenografts not threaten organ donation and call into question the current regulations which protect the activity from the laws of the market? Because a transgenic pig is expensive – more than €300,000 – and its breeding is the monopoly of two American companies not really driven by the philanthropic spirit. “Hence the urgency, if we do not want to find ourselves prisoners of foreign economic interests, to find public funding to ensure European sovereignty”invite Olivier Bastien.
Montaigne versus Descartes
Finally, there remains the question of social acceptability which brings into play the most spectacular dimension of xenotransplantation: that which redraws the border between man and animal. “Does there exist between the two a difference of degree as Montaigne thought, or a difference of nature as Descartes maintained? These two major models of thought serve as a backdrop to the debate on xenografts”deciphers the philosopher Jean-Michel Besnier.
“Be careful not to intellectualize the issues too much, warns Olivier Bastien. The symbolic aspect is important, but what patient will refuse an animal organ if it could save their life? » An argument that Jean-Michel Besnier does not neglect. “Between fascination with technical progress and distrust in principle, the ethical debate serves to find the right balance. »
——
A century of xenografts
In 1906, Mathieu Jaboulay, a doctor from Lyon, transplants a pig kidney and a goat kidney into two patients who survive a few days.
During the 1960s, in the United States, first trials of chimpanzee kidney transplants on thirteen patients. One of them will survive nine months.
In 1983, in California, Stéphanie Fae Beauclair, an infant nicknamed “Baby Fae”, survives twenty-one days with the heart of a baboon.
In 1992, in Pennsylvania, first baboon liver transplant on a patient who died after seventy days.
In 2021, first transplants of genetically modified pig kidneys on two brain-dead patients by the team from Langone Hospital – New York University. Survival time: 74 and 54 hours.
On January 7, 2022, David Bennett, 57, becomes the first transplant recipient of a transgenic pig heart. He died two months later.
On March 16, 2024, Richard Slayman, 62, is the first living patient to be transplanted with a genetically modified pig kidney. He died in May.