Nature is one of the most impactful scientific journals in the world. This is why, when the Conicet researcher, Gabriel Vinderola, was asked to be part of the five members of the jury experts of the 7th edition of the global competition organized by this publication, he did not hesitate to accept.
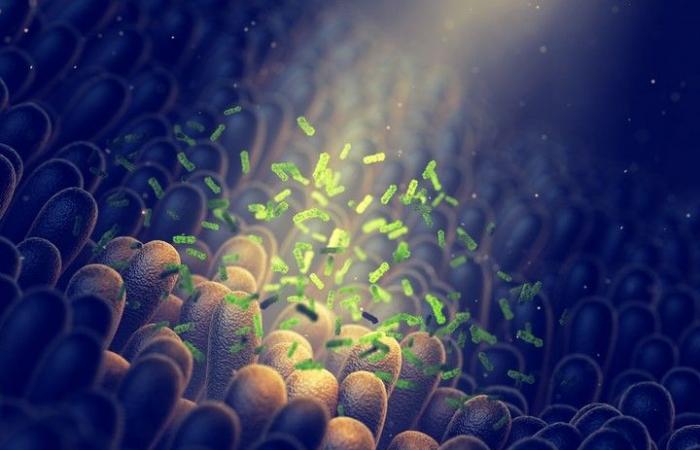
His career demonstrates his expertise in the study of microbiota, a field he has explored for several decades. This complex sphere, populated by microorganisms, mainly inhabits our intestines but is also found in other systems, such as the skin.
This is a growing sector. “Every year, approximately 10,000 research works are published. What we know about the microbiota is only a tiny part, but it is enough to raise awareness, establish behaviors, and analyze what we eat, how we are born, and how we take antibiotics“, Vinderola told Clarionresearcher at the Institute of Industrial Lactology (INLAIN, CONICET-ULN) and teacher at the National University of Litoral.
For Nature’s call for projects entitled “Global grants for gut health”150 research projects on fungi, yeasts, viruses and other lesser-known forms such as archaea were submitted. The study of bacteria was excluded this edition, “because we already have enough information, we wanted discover other realms and their interactions to determine our health,” explained the Argentine researcher.
Two key moments
— What certainties do we have about the microbiota?
— What we know is considerable and communicable with certainty. We know that the microbiota influences our health and that it forms our immune system. In addition, there are behaviors to adopt and mistakes to avoid. In fact, we can count on one hand the essential practices for the proper functioning of our microbiota and our immune system.
I always divide these practices into two main moments: the first concerns birth and the first two years of life. It is at this stage that the “cards” of the microbiota are dealt out.
— What determines whether good or bad “cards” are received during this sharing?
— Major factors include type of delivery, breastfeeding and antibiotic use. In some places, 70% of children are born by cesarean section, less than 50% receive breast milk, and more than 40% take antibiotics in the first year of life; these three elements are harmful to the microbiota.
— What does “harmful” mean and what is the consequence?
— This helps us understand the increase in allergies, inflammatory diseases, childhood diabetes, and even autism. Our genetics have not changed as humans, what has evolved is our microbial genetics: the microorganisms we should have are missing, mainly due to this combination of factors: cesarean deliveries, poor breastfeeding and excessive use of antibiotics.
— Is one of these factors more impactful?
— Breastfeeding significantly corrects dysbiosis (i.e. alteration of the microbiota) caused by cesarean section and antibiotics. If a child needs to be given antibiotics, we have no other choice. However, the power of breastfeeding to restore balance is immense. This is why it is essential to raise awareness and create spaces to promote it.
Lactation should not be considered solely the mother’s responsibility; it is also a social problem. The family, the environment and the system must allow the mother to remain close to her baby. We must change this social outlook that pushes women to breastfeed in secret. The breastfeeding process requires immense effort and should be completely normalized; no mother should feel ashamed of it. As a society, we still have a long way to go.
— You mentioned two big moments: this is one, the one that comes with our heritage and the possibility of correcting it through breastfeeding. What about the second?
— The second moment is when we introduce complementary food, that is to say from the age of six months, when we begin to offer other foods. It is at this stage that eating habits are formed, offering a great opportunity to favor fresh foods, rich in fruits and vegetables, and in varied colors.
And later, as we grow up, we have the responsibility to choose what we eat. We eat three or four times a day, which determines our microbiota and, therefore, our health.
How to maintain a good microbiota
— What foods promote a good microbiota?
— A healthy base should consist of seasonal fruits, vegetables and produce, whole grains and legumes. Additionally, it is essential to consume fermented foods because they contain live bacteria, such as yogurt with probiotics. A balanced diet helps prevent the majority of chronic diseases via the microbiota.
— What foods should we avoid?
— It would be better to limit ultra-processed foods, which are not only problematic because of excess sugar, salt, trans fats, colorings and additives, but also because they lack fiber , essential to our microbiota. The real problem with ultra-processed foods is their lack of fiber.
Ancient hunter-gatherers consumed about 150 grams of fiber per day, spending their time harvesting and consuming fiber-rich, energy-poor foods. Currently, we have a big gap to fill.
—How sick are we?
— The recommended fiber consumption is between 25 and 40 grams per day, while the population average does not exceed 8 to 10 grams. We are far below. 90% of people consume less than half of the necessary fiber. We have a food debt, a debt to our microbiota, which we can repay with the foods we neglect.
— In addition to this food debt, what other factors harm our microbiota?
— Another major problem is self-medication: we take antibiotics and antacids for any reason, when this should only be done under medical prescription. We exercise less than recommended and we don’t get enough rest. It is our way of life as a whole that needs to be revised.
— We know that one of the side effects of antibiotics is the elimination of beneficial bacteria in the intestines. What is the risk of misusing antacids?
— Our digestive system has an acidity gradient: it is very acidic in the stomach and becomes more neutral towards the colon. If I modify this gradient by taking an antacid, it also impacts the acidity of the downstream areas. This causes a sort of shift: bacteria that previously grew in the colon move toward the small intestine. This is one of the causes of what we now call SIBO (Small Intestine Bacterial Overgrowth). The abuse and chronic consumption of antacids are one of the origins.
— Are there ways to know how healthy our microbiota is?
— Microbiota examinations are very useful in the context of a clinical trial, but not at an individual level. There is a huge proliferation of microbiota tests, but their clinical validity is low, there is no international consensus, because the microbiota varies greatly from person to person. We have not yet been able to define what constitutes a normal microbiota. By analyzing 100 healthy people, I will obtain a specific profile. By examining 100 other healthy people, I will obtain a different profile. And even if I reanalyze the same individuals in a month, the profile will change.
If I do a blood test and your cholesterol is 500, I can conclude that you have a cholesterol problem. If vitamin D is below a certain threshold, I can also diagnose a deficiency. But for the microbiota, there are no established parameters yet, and it will be difficult to establish them in the future.
Currently, it is not possible to define, from a stool sample, which profile constitutes a healthy microbiota. What prevails is clinical observation. How do I know if my microbiota is healthy? If I do not have gastrointestinal symptoms or skin problems, because certain dermatological pathologies can be linked to dysbiosis. Before analyzing my microbiota, I need to examine my lifestyle, which can give me an indication of the state of my microbiota.