Étude PHARM-HF A&F – D’après la présentation « Evaluation of randomized audit and feedback to increase heart failure medication optimization among primary care pharmacists in the veterans affairs health care system” – Alexander Sandhu (Cardiologist, Stanford University in Palo Alto, California), Alexandra Steverson, Anju Sahay, Parisa Gholami, Regina Godbout, Scott Mambourg, Jennifer Marin, Kushal Shah, Shoutzu Lin, Tomasz Jurga, Hayden Bosworth, Paul Hess, Paul Heidenreich
Evaluation of Randomized Audit and Feedback to Increase Heart Failure Medication Optimization Among Primary Care Pharmacists in the Veterans Affairs Health System.
Key messages
- PHARM-HF A&F shows that it is possible for pharmacists to further optimize HF treatments recommended by the recommendations
- Education, training and support can be 1st steps to begin to transform HF management practice by pharmacists
- This support by pharmacists makes it possible to increase access to HF care without waiting for the patient to present with an acute HF picture.
- Audit and feedback slightly improves HF patient visits compared to education alone
Introduction
In this study, called the PHARM-HF A&F Study, researchers provided Veterans Health Administration (VHA) pharmacists with educational resources and feedback on the care of patients with HF to assess the impact on improving care. It should be noted that in the VHA, pharmacists can provide medication advice, follow-up and independently prescribe therapies, explains the study’s lead author, Alexander Sandhu. The study was funded by the American Heart Association Rural PRO-CARE Health Equity Research Network and the Veterans Affairs QUERI Program.
Assumption
The prescription of optimal medical treatment of insufficiency (CI) guided by recommendations remains suboptimal. Previous trials have demonstrated that pharmacist support improves HF treatment utilization. However, this support remains rare. The authors hypothesized that auditing and feedback (“FeedBack”) on the care provided to patients suffering from HF could enable optimization of HF medications by pharmacists.
Method
One hundred and twenty Veterans Affairs (VA) pharmacists responsible for 7,378 HF patients participated in the study. The pharmacists were randomly distributed (1:1:2) into three groups: “Audit” and “Feedback” (AεF), AεF with targeted patient information (AεF+) and usual care with education (UC).
In the 3 groups (UC, AεF, AεF+), pharmacists received monthly one-hour interactive webinars during which medical therapy for HF was discussed. A website was available that included titration protocols, best practice documents, and a database of questions and answers on medication management in HF.
The AεF and AεF+ groups also benefited from a monthly email indicating the number of IC treatment actions carried out compared to the other pharmacists in the study, the rate of patients presenting optimal IC treatment (according to the guidelines) at their center level. The AεF+ group also received a list of 7 patients from their center who could benefit from optimization of their HF treatment.
The aim of the study was to assess whether providing pharmacists with training on HF, and data on how often they adjust HF medications compared to their peers, increases the frequency of adjustments in HF medications versus HF education alone.
Primary endpoint : The primary outcome was the difference in HF medication adjustment rate between the combined AεF/AεF+ and UC groups 3-6 months after randomization.
Results
Out of 120 pharmacists, 28 pharmacists were randomized to the AεF group, 30 pharmacists to the AεF+ group and 62 pharmacists to the UC group. Before the intervention, each pharmacist had an average of 2.1 consultations per month related to HF and 0.4 consultations related to medication titration for HF.
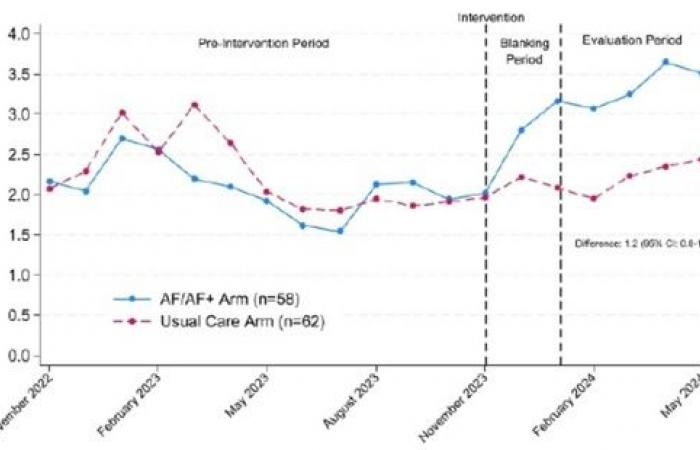
Regarding monthly visits (Figure 1): pharmacists randomized to UC had 0.5 (95% CI: 0.0-0.9) additional monthly visits related to UC. Pharmacists randomized to AεF/AεF+ had 1.2 (95% CI: 0.8-1.7) additional monthly visits related to IC. There were no significant differences between the AεF and AεF+ groups (0.1; 95% CI: -0.6 to 0.8).
Figure 1 : shows the evolution of monthly visits related to IC between pharmacists in the AεF/AεF+ groups and those in the UC group. There were 1.2 additional monthly meetings (95% CI: 0.8-1.7) related to IC in the AεF/AεF+ groups during the evaluation period compared to the UC group.
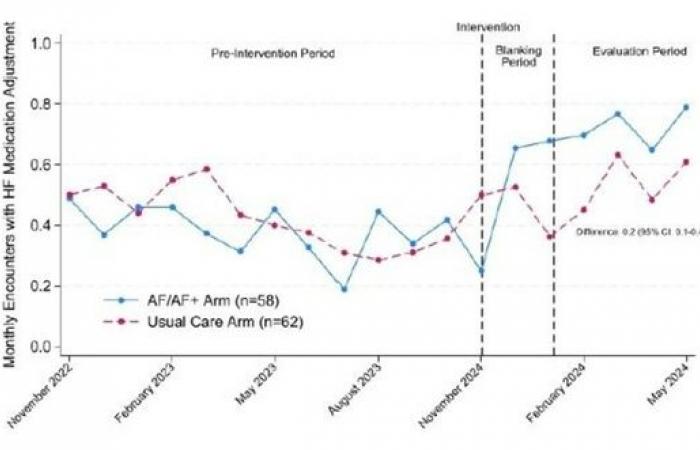
Regarding the optimization of processing (Figure 2): pharmacists randomized to AεF/AεF+ had an increase in monthly visits with therapeutic optimization compared to the UC group (0.2; 95% CI: 0.1-0.4).
Figure 2 : shows the change in monthly visits with adjustment of IC medications between pharmacists in the AεF/AεF+ groups and the UC group. There were 0.2 more monthly meetings (95% CI: 0.1-0.4) with medication adjustment for HF in the AεF/AεF+ groups during the evaluation period compared to the usual care.
The AεF/AεF+ group was more likely to prescribe mineralocorticoid receptor antagonists (11.3% vs. 9.0%; p=0.01). There were no other significant differences in medication prescriptions for HF.
Conclusion
Dr. Jackevicius emphasizes in the discussion that the follow-up period was short (6 months) and that an additional follow-up period would be interesting. She also noted that site-to-site variations were significant. Patient, pharmacist and site characteristics that were associated with better HF management and therapeutic optimization need to be defined. She also noted that this study applied to a specific population (military veterans) and that further studies would be needed to apply it to other populations.
Dissemination of educational resources and feedback on the care of patients with HF is an effective approach to increase optimization of HF therapeutics by pharmacists.
Reference
The AHA presents information for the general public about HF online: Signs and symptoms of HF, View an animation about HF
All the latest news from the AHA