Biomedical prevention and the paradigm shift it has caused have made it possible to strengthen the preventive offer. This now includes screening, condoms, but also post-exposure treatment, preposition prophylaxis (PrEP) and treatment as prevention for people living with the condition. HIV Human immunodeficiency virus. In English: HIV (Human Immunodeficiency Virus). Isolated in 1983 at the Pasteur Institute in Paris; recent discovery (2008) rewarded with the Nobel Prize in Medicine awarded to Luc Montagnier and Françoise Barré-Sinoussi.
In this evolving context, it is more important than ever to assess the appropriation of all of these tools in a population that is still disproportionately affected by the HIV epidemic: men who have sex with men, THE MSM Man having sex with other men. This is the aim of the Sex Report (ERAS) 2017, 2019, 2021 and 2023 surveys, the results of which allowed Annie Velter and her team at Public Health France to estimate the preventive coverage of this population. This new indicator was presented by the researcher on the occasion of the 2024 sexual health days, organized by the SFLS, the SPILF and Public Health France.
ERAS, since 2017, is a cross-sectional, repeated, anonymous, online survey, based on volunteering, set up by Public Health France, with the support of ANRS-MIE. A website is entirely dedicated to this survey and allows volunteers to answer a questionnaire online, from February to March or April. Recruitment of participants has evolved a little since 2017; it is now done exclusively digitally. Banners, formerly on gay dating sites, are now placed on geolocated applications, but also on community information sites. The banners are also distributed on social networks to adult men with a certain profile, despite the difficulties of targeting on these platforms. The questionnaire, self-administered, is rather short, even if the number of questions has increased over time. It collects socio-demographic characteristics, information on lifestyles, health, and obviously, sexuality, preventive behaviors, whether with regular or occasional partners, in the last six months before the survey and during of the last sexual intercourse.
During its four editions, ERAS brought together a huge number of participants, with more than 83,000 participants completing the questionnaire. Among them, only respondents indicating that they reside in France, and meeting the definition of MSM (having already had sexual intercourse with a man), but also who declared having had at least one occasional partner in the last six months, were taken. taken into account for this analysis. The results presented relate to more than 44,000 participants, 10,192 for 2017, 12,901 for 2019, 7,752 for 2021, and finally, 13,219 for 2023. This new indicator takes into account all respondents, regardless of their serological status.
Assess exposure to HIV based on sexual practices
Six mutually exclusive categories of participants were highlighted. The first four were considered to have sexual practices that could not transmit HIV:
- people, regardless of their HIV status, who have not practiced anal penetration with their casual partners;
- people, regardless of their HIV serological status, who have practiced anal penetration while systematically using condoms;
- people living with HIV with viral load The plasma viral load is the number of viral particles contained in a blood sample or other container (saliva, CSF, semen, etc.). For HIV, viral load is used as a marker to monitor the progression of the disease and measure the effectiveness of treatments. The level of viral load, but even more so the CD4 count, contributes to the decision to treat with antiretrovirals. undetectable thanks to treatments that practiced anal penetration unprotected by a condom with occasional partners;
- People who have had anal penetration without a condom but protected by Prep Pre-Exposure Prophylaxis. PrEP is a strategy that allows an HIV-negative person exposed to HIV to eliminate the risk of infection, by taking, continuously or “on demand”, anti-retroviral treatment based on Truvada®. with occasional partners
The last two categories are considered to have sexual practices that put them at risk of HIV infection or transmission:
- HIV-positive people without treatment or with a detectable viral load practicing anal penetration without a condom with casual partners;
- People who are HIV negative or untested, who are not on PrEP, and who practice anal penetration without a condom with casual partners.
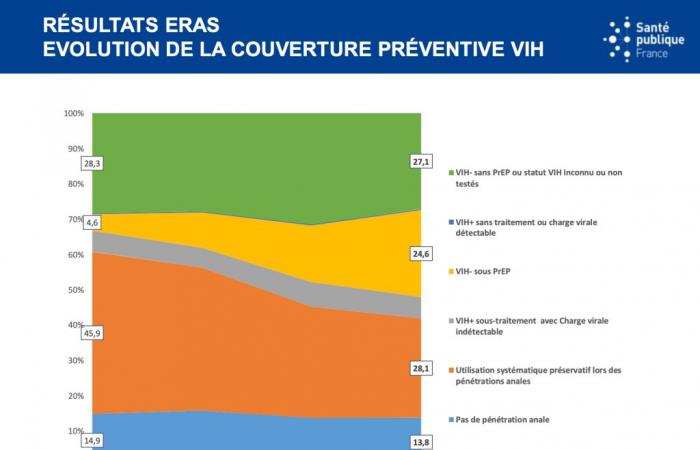
Stable preventive coverage
According to Annie Velter, preventive coverage has not increased much between 2017 and 2023, and goes from 71% to 73%:
- The proportion of people who do not practice anal penetration is stable at around 15%;
- Systematic use of condoms has declined sharply, from 46% to 28%;
- This drop is offset by the share of HIV-negative MSM on PrEP, which increases significantly, from 5% to 25%;
- The proportion of people living with HIV on treatment with an undetectable viral load remains stable at 6%.
Let us note in passing that the number of intercourse without penetration varies little, whether according to time, age, place of residence or sexual orientation, whether exclusive or not, although this practice is not specifically valued in prevention.
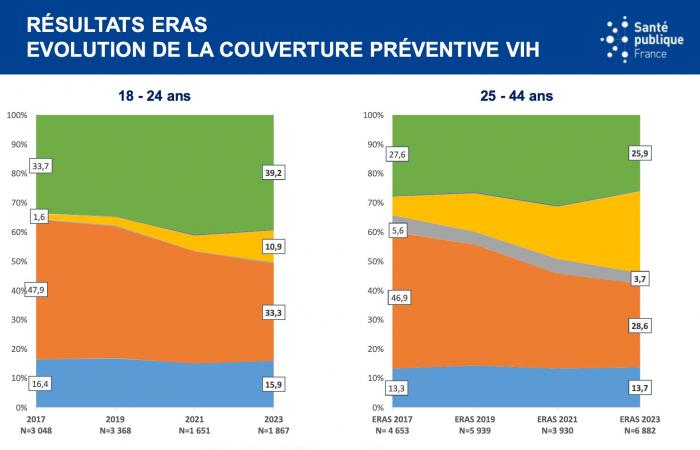
This development varies according to age groups: among 18-24 year olds, where we actually see a reduction in the use of condoms with occasional partners (from around 48% to 33% of participants), but the use of PrEP increases little (1.6% to 10.9%) and sexual practices exposing a risk of HIV infection in 2023 represent 40% of sexual relations in the last 6 months. Among 25-44 year olds, the share of PreP is 28% to the detriment of condoms, and non-protection of penetrative sex remains 26%.
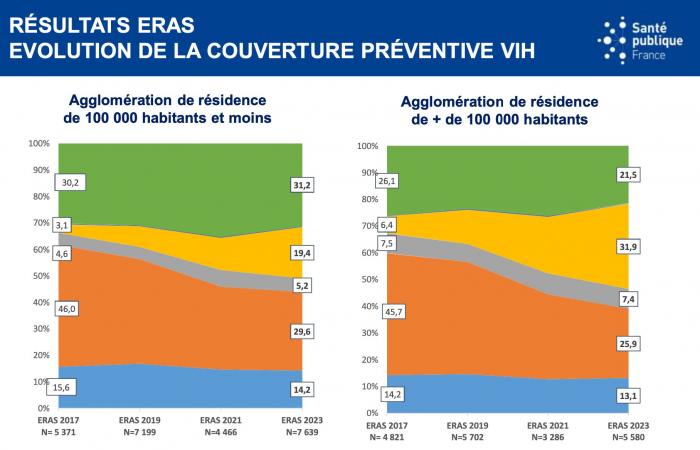
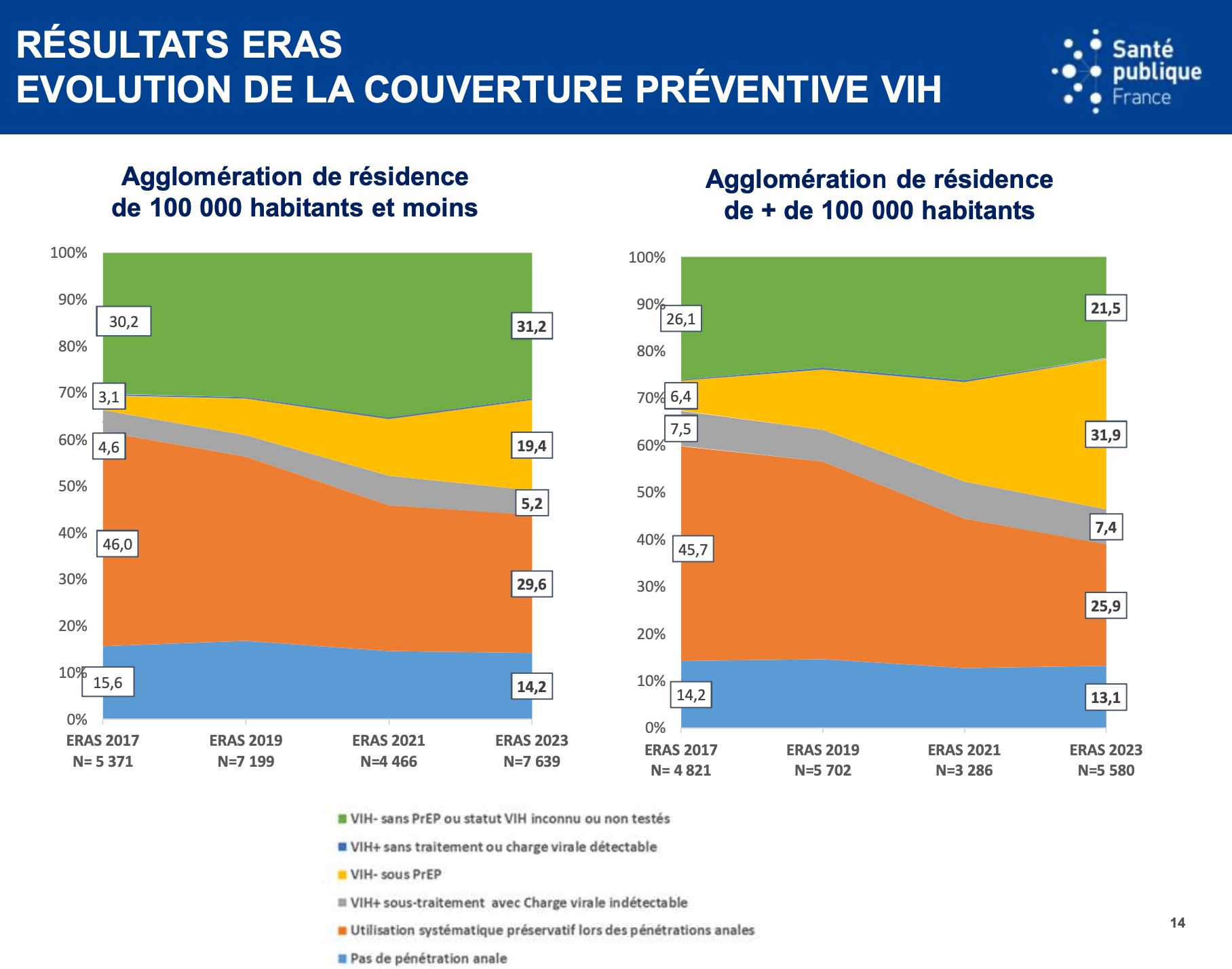
We also see a difference depending on the declared place of residence: MSM residing in a town of less than 100,000 inhabitants protect their penetrations less (31% VS 21% for those residing in a large urban area), still with this differential on the use of PrEP and the systematic reduction in condom use.
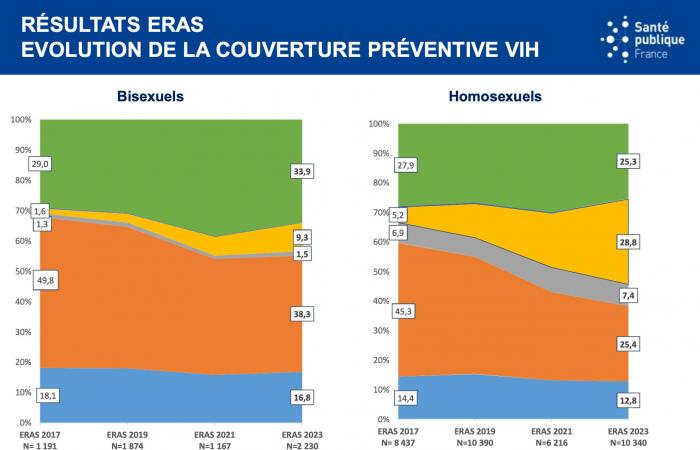
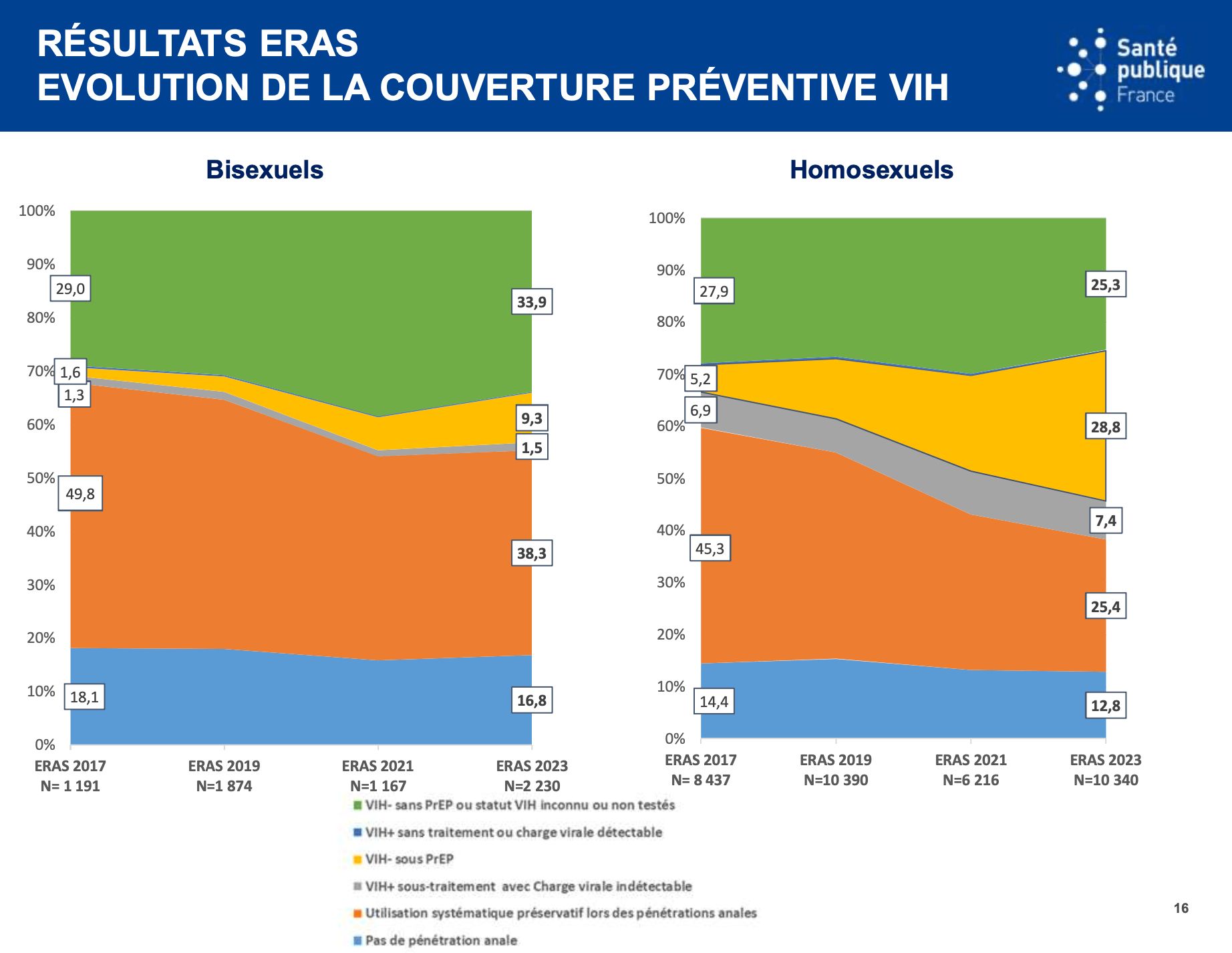
And finally, only 9% of MSM declaring themselves bisexual use PrEP, compared to 29% of homosexuals, with a level of non-protection estimated at a significant level, 34%.
Profile of participants in the ERAS survey
The participants are mainly men born in France: there are very few men born abroad among the participants (around 6%), and the majority of them were born in a European country; which suggests a participation bias even though we know that MSM born abroad outside Europe constitute a group whose number of new diagnoses is not decreasing. The level of higher education at the BAC is also important, from 68% to 75% of participants. They are urban, even if we see a decrease in people residing in large cities (47% to 42%). Finally, this is a sample that is in a fairly comfortable financial situation (53% to 64%).
The researcher also noted an aging of the population participating in this survey – a classic phenomenon in repeated surveys -: we go from 31 years on median in 2017 to 38 years in 2023, with a proportion of those under 25 going from 30% to 14%.
The participants are predominantly homosexual (around 80%), with a slight increase in the proportion of people declaring themselves bisexual (from 12% in 2017 to 17% in 2023). Most frequent gay friendly places (around 70%) and have had several partners in the last 6 months: more than 10 for 26% in 2017, 30% in 2023.
The figures for the use of screening are encouraging, even if still insufficient, since it increased significantly between 2017 and 2023, from 56% to 64%.
Comparable results in several countries
Annie Velter recalled that these results are not representative of the entire MSM population in France, but that the ERAS system makes it possible to obtain a solid sample, with diversified profiles, despite a notable aging of the participants.
The results are also similar to those presented by foreign colleagues, in particular those of Martin Holt for Australia, who reported preventive coverage of around 75% for 2021, a figure close to the 73% observed in France. However, there is a notable difference: The preventive coverage offered by PrEP is 35% in Australia, which partly explains the excellent results that the country has been able to boast of in recent years.
Finally, the different results obtained according to age, according to place of residence or even between bisexuals and homosexuals need to be better explained and confirm the importance of looking for ways to offer or make available prevention adapted as much as possible to sexual behaviors.