The era of miniaturization in medicine is in full swing and is poised to revolutionize the way things are done. An international conference on the subject, which took place last week in Montreal, testifies to the dynamism of this booming discipline which aims, among other things, to reproduce human organs on a chip, to design portable and rapid diagnostic tests, and even to develop small portable devices capable of continuously measuring different physiological parameters, such as sweat and its composition in order to indicate to athletes when to hydrate.
During the International Conference on Miniaturized Systems for Chemistry and Life Sciences — MicroTAS 2024, we were able to discover the most recent advances in mini-laboratories on a chip which make it possible to analyze biological liquids with the aim in particular of make a diagnosis.
This discipline aims “miniaturization, so that [ce mini-laboratoire] can be used easily anywhere, so it requires less sample quantity — instead of taking a blood sample, just one drop will be enough. This miniaturization also makes it possible to speed up certain processes and reduce the time required to obtain the result,” explains the co-president of the conference, David Juncker, from the outset.
This professor in the Department of Biomedical Engineering at McGill University gives the example of rapid tests to detect COVID-19, which are in fact mini-laboratories on which a sample taken from the bottom of the nasal cavity is placed and which render a diagnosis within 15 minutes. Whereas with PCR tests, we had to go to a specialized center to take the sample and we received the result one to two days later.
In collaboration with microbiologist-infectious disease specialist Donald Vinh, from the McGill University Health Centre, Mr. Juncker’s team has notably developed a laboratory on a chip making it possible to measure antibodies involved in the inflammation process in a drop of blood. and which predict whether an individual is at high risk of severe COVID-19. “Among men over 65, those who have a large concentration of these rogue antibodies have a higher risk of severe COVID-19 requiring hospitalization, and even mortality. The idea is that if a person in this category tests positive for COVID, we would use this chip to detect these antibodies. And if a large quantity is found, he could be given the antiviral Paxlovid right away to reduce the risk of him developing a serious illness. With our device, we could obtain the results in around half an hour, whereas the result of a traditional test arrives too late to intervene,” argues Mr. Juncker.
These labs on a chip are evolving at great speed. Some researchers have even designed them in the form of portable devices, such as flexible adhesive strips (patch) which is applied to the skin. A well-known commercial example adopted by athletes is the Gatorade Gx Sweat Patch, which measures sweat secreted over time, as well as the amount of salt and electrolytes it contains, and signals to the athlete when and how rehydrate.
Professor John A. Rogers of Northwestern University in the United States is a pioneer of these flexible electronic devices that can be stuck to the body to perform various measurements, usually carried out by hospital equipment. His team worked to adapt this wireless, battery-free technology for monitoring premature babies, who are normally connected by multiple wires to machinery measuring their vital signs. Different sensors are stuck on the bodies of infants: mechanical-acoustic sensors which record heartbeats, respiratory rate and blood pressure; optical sensors that assess blood oxygenation; fluidic sensors that detect biomarkers contained in sweat and provide information on blood chemistry; electrical sensors that measure body temperature.
At the Montreal Children’s Hospital, we are experimenting with this monitoring system which transmits information wirelessly directly to the computer system in the intensive care unit. Babies are no longer harnessed as before, parents can now hold them in their arms. “These sensors continuously monitor breathing parameters, in particular, which allows us to know whether the newborn is ready to be extubated. Until now, it was the doctor who decided to carry out this intervention. If he was wrong, we would have to reintubate the baby, which is a very invasive procedure that we want to avoid as much as possible,” emphasizes Mr. Juncker.
The other major field of research presented at the conference concerns human organs on a chip. “From your cells, we create some of your tissues, which we can then use to understand fundamental principles of physiology and pathologies, or to test drugs,” summarizes the co-president.
Thus, researchers have succeeded in creating hearts-on-a-chip composed of cells that beat autonomously and on which drugs for arrhythmia are tested. Others cause mini-cardiac arrests on-chip and then attempt to regenerate the destroyed cells.
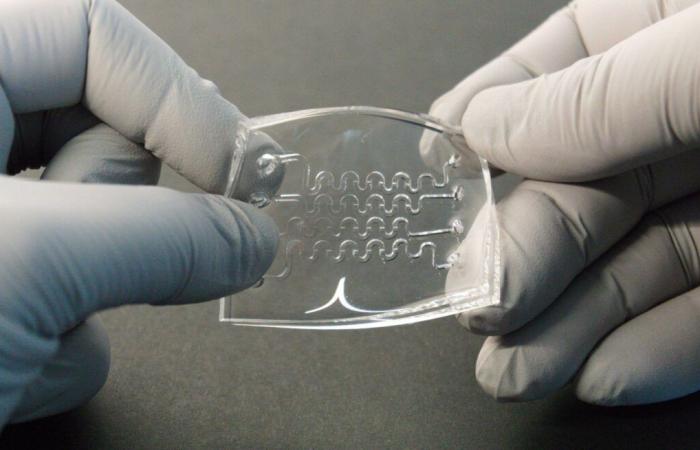
Most of the time, we do not recreate the organ in its entirety, but only the key components allowing us to reproduce the function we wish to study. In these organs on a chip, there is nothing electronic, it is the structure of the organ that creates the function. We guide the formation of this structure by creating microscopic channels to ensure communication between cells, explains Thomas Gervais, professor at Polytechnique Montréal and researcher at the CHUM Research Center, who co-chairs the local organizing committee for the congress.
Other researchers thus imitate the functioning of brains, kidneys, colons and livers on a chip. Several teams of scientists are developing blood vessels with the aim of studying the barrier that they erect between the blood and the brain, and which often prevents drugs from entering the brain, where they would have a role to play. “This blood vessel-on-a-chip model makes it possible to check whether or not a drug will penetrate the patient’s brain, and thus to know whether it will be worth carrying out in a clinical trial. This type of device is worth gold for the pharmaceutical industry, which thus saves time and money,” explains Thomas Gervais.
From your cells, we create some of your tissues, which we can then use to understand fundamental principles of physiology and pathologies, or to test drugs.
Mr. Gervais’ team cultivates pieces of ovarian cancer tumors taken from patients. On these half-millimeter samples containing up to 20,000 cells, she tests the therapy that is planned to be administered to a patient. “If this therapy does not seem effective on the chip, we will not give it to the patient and we will immediately consider another treatment, which will avoid wasting time and subjecting the patient to exhausting side effects,” underlines the scientist.
Some researchers are working to connect different organs on the same chip using tiny pipes acting as a circulatory system. “It is not to create living beings on a chip, but to create the simplest, but most representative model of a human being possible,” says Mr. Gervais. Some are currently able to produce systems including a liver model and a cancer tumor in order to simulate the effect of a drug even more faithfully. Because many drugs are not active until they have been metabolized by the liver.
These organs on a chip are now highly prized tools in medical research. The United States Food and Drug Administration (FDA) even adopted the Modernization Act 2.0 in December 2022, which allows the use of these organs on a chip to replace animal testing to obtain authorization to carry out trials. clinics.