By studying the behavior of the respiratory microbiota of patients during bacterial pneumonia, the Phenomenon project hopes to identify bacteria or probiotics which would be administered to patients to improve their chances of recovery.
An article to be found in Inserm magazine n°60
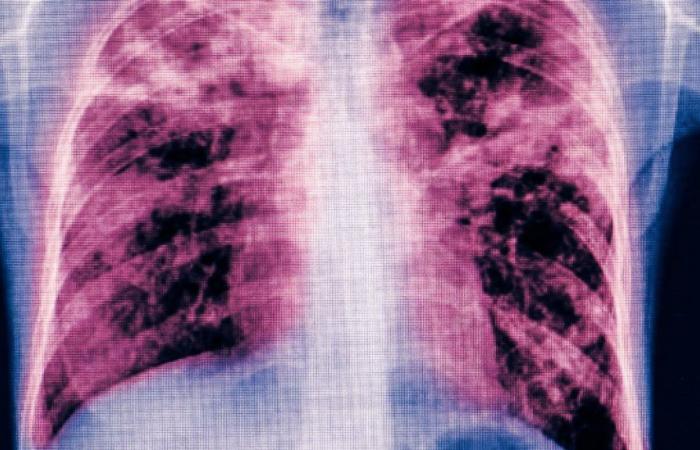
Despite progress in the management of bacterial pneumonia, around a third of the 500,000 cases treated annually in hospital end in treatment failure. The introduction of new antibiotics will be insufficient to counter this observation, when we know that bacteria sooner or later end up becoming resistant. It is therefore a completely different paradigm that must be developed today to better cure these pulmonary infections. Researchers from the Phenomenon project, set up in the summer of 2023, believe that the answer lies in the patient’s respiratory microbiota. “ It was long believed that the lung was sterile and that pneumonia resulted from its infection by an isolated pathogen.explains Jean-François Timsit, one of its founders. We now know that our respiratory tract is colonized by a community of so-called “commensal” bacteria, which live in harmony and regulate the immune response of our airways. When treating a respiratory infection, the local balance is upset. Our research will allow us to understand how these disturbances lead to therapeutic failure. »
Does the germ or the antibiotic cause the disappearance of one or more commensal bacteria, beneficial to the pulmonary microbiota? Do they disrupt their metabolism? The project will explore these different avenues with two main objectives: to identify changes in the composition or function of the respiratory microbiota which are associated with therapeutic failure, and to find new treatment avenues. “ It is an extremely ambitious project, in a little-known fieldcomments Jean-François Timsit. The difficulty will consist of sorting through the statistical associations that will appear between the state of the microbiota and the state of the patient, in order to find those for which there is a cause and effect link. »
Bacteria, potential treatments for infection?
As part of the European HAP project2Antoine Roquilly in Nantes studied the genetic expression (microbiome) of the respiratory microbiota, and showed that the reduction in the abundance of four bacteria was associated with severe pneumonia requiring respiratory assistance. In the context of Phenomenon, he wishes to go further: “ Now that we have identified these species, we will study the metabolic functions that they provide and how these fluctuate with the clinical outcome of the patient. » He also wishes to repeat the same work for less severe pneumonia. To do this, he will use bacterial samples obtained from four cohorts of patients that Jean-François Timsit and his team are currently establishing in Nantes and Paris. “ Each brings together different profiles: mild pneumonia treated on an outpatient basis, pneumonia acquired in the community requiring hospitalization, severe pneumonia acquired in the community and admitted to intensive care, and severe nosocomial pneumonia admitted to intensive care. » Samples will be taken from the pharynx and bronchi at the start of the disease, during antibiotic treatment and in the event of therapeutic failure. The diversity, richness and function of the microbiota will be analyzed, compared to healthy subjects. Furthermore, from these samples, the analysis of gene expression and that of small molecules produced by local metabolism will make it possible to establish what functions of the microbiota and, secondarily, what functions of the host’s immune system are modified during infection.
“ In a second part, we will validate the results in animals by studying more precisely the bacterial species or the metabolic pathways which have been described as interesting. », explains Antoine Roquilly. Ultimately, this work could lead to new therapeutic perspectives: if it appears that the disappearance of a bacterial species is harmful to healing, reestablishing its presence could help fight the infection. The idea of injecting bacteria into a patient to treat pneumonia could then become a reality. “ We can imagine that we will test the respiratory microbiota of patients during their hospitalization for pneumonia, before initiating antibiotic therapy.suggests Jean-François Timsit. Those who have a microbiota at risk of unfavorable outcomes could receive probiotics, by aerosol or orally. People at risk of pneumonia, such as the elderly, could even be prescribed preventive probiotics aimed at stabilizing the respiratory microbiota. »
Resistome: friend and foe
The good bacteria usually present in the respiratory microbiota of patients can naturally possess antibiotic resistance genes: this advantage allows them to not disappear during treatment. However, if these resistance genes were transmitted to pathogenic bacteria, through a phenomenon called “gene transfer”, the latter would in turn be resistant to antibiotics…” For the moment, there is little data on the subject, but the probability that a resistance gene is transferred from one bacteria to another is generally higher when the two bacteria are structurally close. », explains Étienne Ruppé, also a researcher within the unit Inserm Infection, antimicrobials, modeling, evolution. Using samples from the different cohorts, the scientist characterizes all the resistance genes (or resistome) of the microbiota, and evaluates whether the presence of one of them is associated with lower chances of recovery from pneumonia. In this case, the possibility – and the mechanisms – by which gene transfer takes place from commensal bacteria to the pathogen will need to be characterized. Analysis of the resistome could therefore lead to the identification of commensal germs whose genome is beneficial to maintaining lung function during the treatment of pneumonia. After identifying the resistance genes, Étienne Ruppé will synthesize the corresponding proteins to better understand how and to which antibiotic they enable resistance. “ These species could then be used as probiotic at the time of antibiotic therapyhe continues. But because the bacteria of the respiratory flora are often difficult to isolate and cultivate outside the lungs, others which would protect the previous ones from the action of the antibiotic and which would be easier to handle could also be used as probiotics. » Real bodyguards. In any case, another approach, also innovative, when we know that 60% of deaths from infections in France are due to pneumonia.
Jean-François Timsit and Étienne Ruppé are both researchers in the Infection, antimicrobials, modeling, evolution unit (IAME, unit 1137 Inserm/Université Paris-Cité/Université Sorbonne Paris Nord), Paris.
Antoine Roquilly co-leads the Host-Pathogen Interactions, Inflammation and Mucosal Immunity team in the center of translational research in transplantation and immunology (CR2TI, unit 1064 Inserm/Nantes University), in Nantes.
Author: C.G.
Read also
Antibiotic resistance
Antibiotics have significantly reduced mortality associated with infectious diseases…