The European regulatory authority EMA has approved an antibody preparation for the first time. This is an important step – even if the remedy is controversial.
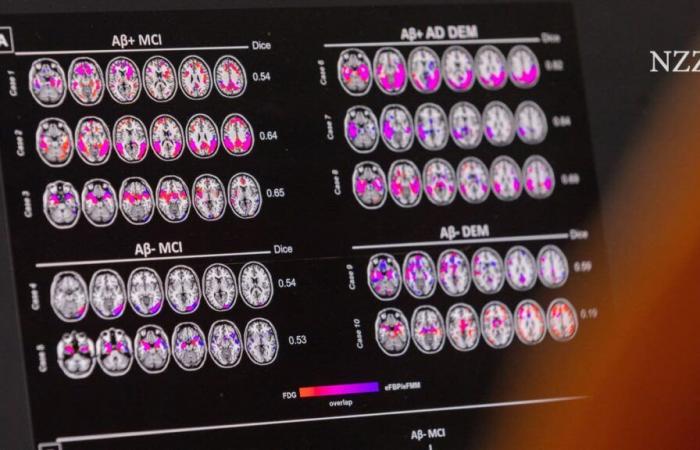
Imaging procedures reveal Alzheimer’s disease: The brain acts like a holey sponge, and some areas no longer receive a good blood supply.
Denis Balibouse / Reuters
Savior? Beginning of a new era? Or a lot of money for little effect? Hardly any drug has been as hotly debated among doctors and patients in recent months as a new drug against Alzheimer’s. It has the somewhat unwieldy name Leqembi. The decisions of the experts at the European Medicines Agency (EMA) are an example of this disagreement. In July they spoke out against approval. On Friday they gave the green light.
The U-turn is correct. The drug can actually usher in a new era of Alzheimer’s therapy.
The remedy slows the progression of the deficits
Because Leqembi is the first drug ever to slow down the steadily progressing Alzheimer’s disease. Some other drugs with similar antibodies can also do this and are also expected to be approved in Europe soon.
Even slowing down dementia is worth a lot. For patients and their relatives, this can mean that those affected can live largely independently for longer. That they will have to go to a nursing home later. That they can still consciously experience important family events such as a golden wedding or the first grandchild.
But Leqembi is not a miracle cure. It doesn’t cure Alzheimer’s. The progression of dementia is only slowed down very moderately. And we don’t yet know how long the effect will last. And it is particularly effective at the beginning of dementia, when the symptoms are not yet too severe.
Currently, no medication can provide a cure. Nobody can yet explain how dementia develops. What is clear is that many factors damage the brain. One of them are protein clumps that stick to nerve cells and poison them. Leqembi’s active ingredient, an antibody called lecanemab, binds to such clumps. These are then disposed of. This slows down cell death. But existing holes will not be repaired. It is also unclear to what extent other harmful processes are stopped by the antibody.
Of course, it is true that given the drama that Alzheimer’s causes for patients and their families, the results achieved so far look disappointing. Especially when you consider that, firstly, the preparation alone costs $26,000 per year. Roughly the same amount has to be spent on medical care and accompanying check-ups. Secondly, Leqembi is by no means harmless; in some cases it has caused a dangerous cerebral hemorrhage.
Pioneer for further drug research
Despite all the shortcomings, the approval of Leqembi in the EU is an important step. Only if the preparation is used on many patients in everyday clinical practice can doctors better identify who should receive it – and who should not. This is the only way to be clear about how long the effect lasts and which dosage is most effective for which patient group.
The EMA’s yes also means that Europe can keep up with other countries in dementia therapy research. Leqembi has been approved in the USA, China and Japan for several months. It has also been available in Great Britain since October, but only on your own account.
Leqembi could open the door to further novel dementia therapies. The first AIDS medications were also pioneers. When they came onto the market in the late 1980s, they initially did not have a long-lasting effect. The diagnosis of AIDS remained a death sentence. Almost ten years later, the real breakthrough in therapy came. Today, AIDS is a disease that can be lived with with medication.