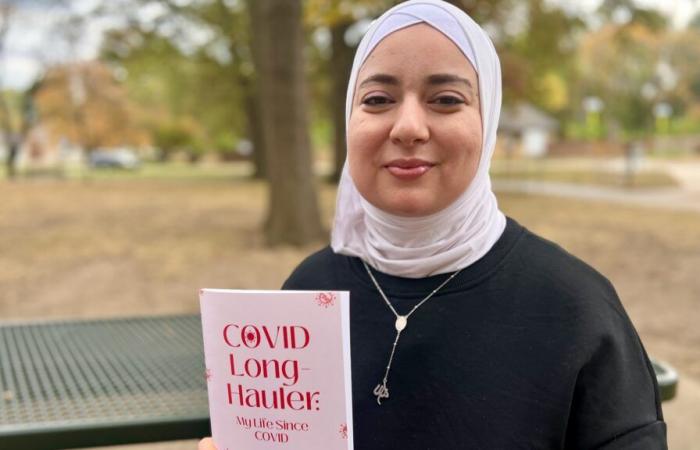
Salam Kabbani wears a smile, and many of her sentences trail into laughter.
That tends to mask the fact that she got COVID-19 three years ago — and never got better.
The 34-year-old Overland Park pharmacist is one of 17 million Americans battling long COVID, an amorphous constellation of symptoms that scientists are only beginning to understand and most doctors are struggling to treat.
Kabbani faced months unable to work. For days at a time, she could barely get out of bed. Just taking a shower exhausts her. She gets dizzy with no notice. Her brain gets foggy. And if she pushes herself even a tiny bit too far, her body simply wilts and she is forced to climb into bed.
“The number of people that are like, ‘Oh, but you look fine,’” Kabbani said, a laugh bubbling to the surface. “Well, yeah, you know, I’m not hemorrhaging from my eyeballs. But I am very much disabled.”
With only 13.5% of adults opting to get the most recent COVID vaccine, a growing number of health care experts and patient advocates are sounding an alarm. The only sure way to avoid getting long COVID, which is believed to affect a third of people infected with the SARS-CoV-2 virus, is to avoid getting COVID.
An up-to-date vaccine, which some people skipped last year, too, is the best way to do that. But public health officials said they face strong headwinds in their efforts to share that message.
Pandemic fatigue and “anti-vax propaganda,” said Dr. George Turabelidze, Missouri’s state epidemiologist, stand in the way. Now Robert F. Kennedy Jr., a known vaccine skeptic, is expected to get a substantial role in Donald Trump’s new administration.
But people shouldn’t be lulled into thinking that COVID will be just like a cold, Turabelidze said.
“Some people — even with mild COVID,” he said, “develop long COVID.”
And long COVID, said Jenna Hopkins, an occupational therapist at University Health, “is ruining people’s lives.”
The U.S. Census Bureau’s most recent household pulse survey found 18.6% of Missouri adults and 16.5% of Kansas adults said they have experienced long-COVID symptoms. Nationally, close to 45 million of the country’s 250 million adults said they have had long COVID at some point.
The illness can take hold of anyone who comes down with COVID, no matter their age, gender or overall health. It can linger for months or years. It can be relatively mild or completely disabling.
And while the severity of an initial COVID infection doesn’t seem to influence whether someone gets long COVID, the number of times a person comes down with COVID could be a factor. In other words, every time you get the virus is another chance to end up with stubborn health problems.
“It gets really ugly very quickly,” said Arijit Chakravarty, a COVID researcher in Massachusetts, “because what it means is that if you wait long enough, everyone is at risk of getting it.”
In bed for a year
If Kelly Meiners could scream from the rooftops to warn people to protect themselves against the virus, she would.
The 49-year-old college professor and marathon runner came down with a relatively minor case of COVID in 2021. She stayed home from the office, even though her symptoms felt like nothing more than a bad cold.
That quickly changed in the weeks after her initial infection cleared up.
“Over the next year, I lay in bed,” said Meiners, who chaired the physical therapy department at Rockhurst University. “I had no idea what was going on with me. I felt I was severely drugged and drunk. I couldn’t make sense of anything. I couldn’t think straight.”
In an effort to fend off debilitating migraines and persistent seizures, Meiners spent most of her time in a dark room, wearing noise-canceling headphones and dark glasses. She couldn’t hold a pen or a fork. She could no longer read or walk.
And when she went to a doctor in Kansas City, she was told that it was all in her head, that she should exercise. As an athlete, Meiners wanted nothing more. So her husband bought a recumbent bike. She strapped herself in and pushed herself until the seizures began.
She was told exercise would make her better. Now she understands it only made her worse.
Finally, a year after falling ill, a friend of a friend got Meiners an appointment at Mayo Clinic in Minnesota. The doctor there immediately knew what was wrong.
“I just cried,” she said. “It wasn’t because there were so many things wrong with me. It was because they finally believed me.”
Finding someone to help
Unfortunately, long-COVID patients often have a difficult time finding someone who can help them. And someone who will believe they are sick.
Doctors didn’t learn about COVID in medical school — let alone long COVID. And they work in a system where they need to document their care for insurance purposes. Long COVID is so new and varied in the ways it shows up, it barely has an agreed-upon clinical definition.
So it’s no wonder some doctors are sending patients away without care or telling them their symptoms are in their heads.
“I don’t think it’s coming from a place of malice,” Kabbani said. “It’s truly just a lack of awareness and understanding and being burned out.”
Now that Kabbani’s health is improved, she spends the extra energy trying to help educate the world about the disease. She has written a book about her own journey, and she and Hopkins, the University Health occupational therapist, are creating a podcast.
Kabbani, who works as an infectious disease pharmacist at Olathe Health, is speaking at continuing medical education events, trying to bring information about long COVID directly to doctors and nurses.
“What I hope to drive home to these providers,” she said, “is that the symptoms are very strange, and they fluctuate. That’s why it may seem like it’s absolutely in their heads. But it’s absolutely not.”
Research theories about long COVID
This summer, long COVID earned a consensus case definition from the National Academies of Sciences, Engineering and Medicine. Someone has the chronic condition, according to the new definition, when health problems are present for at least three months after a COVID infection.
Those problems can affect one or more organ systems, according to the definition, as “a continuous, relapsing and remitting or progressive disease state.” And a person can meet the definition by having just one or multiple symptoms, from the list of 200 included in the definition.
“If people just had lung problems,” said Dr. Adnan I. Qureshi, a professor of neurology in the University of Missouri School of Medicine, “it would be much easier to study.”
The National Institutes of Health launched a nationwide research program in 2021 with a $1.15 billion investment. In February, the agency announced it would spend another $515 million over the next four years.
The program includes dozens of studies and drug trials across the country, including studies at the University of Kansas Health System and Children’s Mercy Hospital.
U.S. Sen. Bernie Sanders of Vermont has introduced legislation that would invest another $1 billion a year for a decade in research, provider education and public education.
Scientists have several theories about how long COVID strikes, and they are starting to believe that there may be more than one answer.
For example, in some cases, the immune system, which has been activated by the initial viral infection, simply doesn’t turn off once the virus is gone. That means a person’s own immune system can damage the body.
Another theory is that when someone has long COVID it could be because they still have traces of the virus in their body.
Another possibility, scientists said, is that the virus damages the circulatory system, which could explain why symptoms are so varied and in so many organs.
Pacing to survive
Doctors are finding that some patients get better over time without treatment. But others need to manage symptoms.
When patients come to see him at University Health’s Center for COVID Recovery, Wesley Strouts, a nurse practitioner who specializes in internal medicine, looks for the symptoms he can treat that will provide some relief. Sometimes he finds different diagnoses to explain what’s happening. Often, he refers patients to Hopkins, the occupational therapist who has built a specialty out of helping patients manage symptoms.
For many patients, Hopkins said, the best approach is to follow “pacing protocols.”
“Sometimes the treatment is the cure,” she said. “When people are able to manage their symptoms … sometimes their symptoms will start to dissipate as long as they are continuing to be very careful to avoid triggering activities.”
For Amanda Finley, 47, who first came down with long COVID after a 2020 bout with the virus, pacing looks like this: Work. Uber home. Straight to bed. Often her weekends must be entirely devoted to sleeping so she can face another work week.
It’s better than the alternative Finley knew in 2021 when she was living in a tent at Weston Bend State Park because she couldn’t work and had no money for rent. The Independence woman couldn’t see her 11-year-old son for months.
But even when Finley had energy for nothing else, she stayed connected with other people dealing with the illness. Early in her diagnosis, she formed a Facebook group for COVID long haulers that today has 16,000 members around the world.
It helps her know she’s not alone. And it could be a tool in science’s effort to solve mysteries surrounding the illness. Finley tries to put researchers in touch with the people in the group.
“The patients are the experts with long COVID,” she said. “We’re the ones going through the jungle with a machete making the path.”
Telling her story
Since her long-COVID symptoms began, Meiners has missed graduations, kids heading off to college, holidays, family vacations and almost every other part of her life.
She just passed the third anniversary of her initial COVID infection, and she still spends 90% of her day on the sofa or in bed. Meiners needs an electric wheelchair to navigate her Leawood home, but with the help of more than 20 prescriptions and pacing strategies to avoid flare-ups, she can have moments with her husband and three kids.
And Meiners has found a small amount of peace in making art, something she’d never tried before this. Her paintings, which tell her long-COVID story, are on display at the Lenexa City Center Library. They have been shown in galleries around the city.
It may not be screaming from the rooftops, Meiners said. But, right now, it’s the best she can do.