EPFL scientists have developed “lymphomoids”. These tumor avatars should make it possible to test the effectiveness of lymphoma treatments in the laboratory and to better predict individual responses.
Cancer is undeniably complex, with each tumor responding to different therapies. This is also the case for lymphomas, a type of blood cancer that starts in lymphocytes, a subgroup of immune cells that help fight infections.
Traditional methods for testing the effectiveness of lymphoma therapies are limited, the Federal Polytechnic School of Lausanne (EPFL) said in a statement on Wednesday.
Tumor avatars
Recently, scientists have begun to develop “tumor avatars”, new systems for preserving cells or tissue samples outside the patient’s body, either ex vivo. However, it was difficult to maintain the original cellular structure and composition of lymphomas.
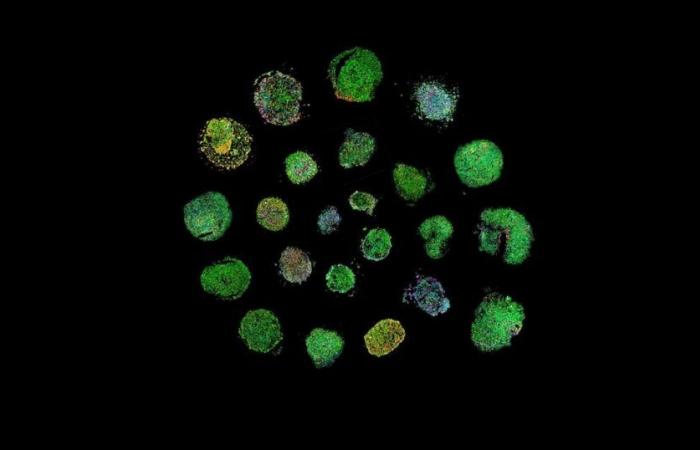
Albert Santamaria-Martínez and Elisa Oricchio, at EPFL, in collaboration with colleagues from CHUV and the University of Lausanne, now present in the journal Nature Communications a more advanced model called “lymphomoid”.
A specific environment allows fragments of lymphoma tissue to be maintained ex vivo for several days. Under these conditions, the architecture, cellular diversity and microenvironment of the tumor could be preserved.
Drug testing
The scientists collected 27 human lymphoma samples and demonstrated, using imaging-based analyzes and spatial molecular profiles, that lymphomoids retain the phenotypic and molecular characteristics of the original tumors.
This made it possible to examine how the samples reacted to different drugs. These reactions closely reflected the clinical responses of the patients whose tissue samples were used.
This research therefore suggests that lymphomoid may serve as a reliable tool to predict individual response to specific treatments. They offer a promising new way to personalize cancer treatment, notes EPFL.
Furthermore, they could also be used in clinical trials to test new cancer therapies and explore the complex dynamics between tumor cells and immune cells during treatment.
ats/sjaq
Health
Canada