It’s a pathology that scares you, and for good reason. Pancreatic cancer is one of those presenting the darkest picture. Only 10 to 15% of affected people are still alive five years after diagnosis. A seriousness which is due to the insidious particularity of this disease, with its considerable metastatic power. “These are very aggressive tumors that grow quickly and quietly,” explains Professor Jean-Louis Frossard, chief physician of the Department of Gastroenterology and Hepatology at the University Hospitals of Geneva (HUG). It is the most perverse of cancers, because its symptoms only appear in the few months preceding death. Among the warning signs: weight loss, pain radiating into the back, sometimes jaundice. Symptoms which remain not very specific.
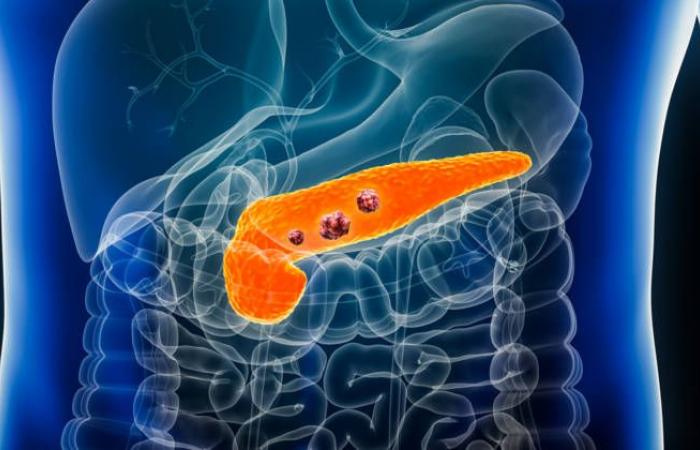
What is the pancreas?
Digestive organ nestled between the spleen and the duodenum, in the upper part of the abdomen, the pancreas is a gland measuring 15 to 20 cm, weighing approximately 50 g. Its anatomical position, at the back of the stomach, makes it discreet and difficult to access. However, it plays an important role in the body, because it interacts with many surrounding anatomical structures. The pancreas indeed participates in digestion by secreting digestive juices containing enzymes. Carried into the small intestine through the pancreatic duct, these allow the breakdown of food so that the body can absorb the nutrients essential to its functioning. From a metabolic point of view, the pancreas is also a key player in the regulation of blood sugar levels. It contains Langerhans cells responsible for secreting insulin, a hormone necessary for regulating blood sugar.
In addition to the sneaky characteristics of this cancer, another point worries specialists: its prevalence. Indeed, recent data shows a dramatic increase in the number of cases in the population, particularly in industrialized countries. In Switzerland, while 4,000 cases were recorded between 1980 and 1984, this figure doubled between 2015 and 2019. And the forecasts are alarming: “Some studies suggest that pancreatic cancer will surpass breast cancer in women in terms of incidence within a few years,” reveals Professor Frossard.
Risk factors identified
A positive fact: knowledge around this disease has evolved considerably in recent years, particularly regarding the causes and risk factors. We now know that advanced age (six out of ten people are over 70 at the time of diagnosis), smoking (30 to 40% of cases are directly linked to tobacco consumption), type 2 diabetes, exposure to certain pesticides particularly in wine-growing regions, or even obesity. It was thus noted that people with a higher body mass index (BMI)[3] At 30, their risk of developing pancreatic cancer increases by 50 to 60%.
Suffering from chronic pancreatitis (read framed), a disease lastingly altering the pancreas, also increases the possibility of this cancer appearing, as does a history in a first-degree family member (father, mother, siblings).
Research that is progressing slowly
One of the major obstacles in the deployment of new therapies and diagnostic methods lies in the fact that, unlike other cancers such as breast or prostate, no tumor biomarker has yet been identified for detection of pancreatic cancer. However, such specific molecules found in cancer cells could facilitate the identification and targeting of tumors. “A biomarker, CA19-9, is sometimes used, but it is not optimal, because it lacks diagnostic performance and is not expressed in all patients,” underlines Professor Frossard.
Among the avenues of research developed, the development of a blood test detecting micro-signals emitted between cancer cells in the bile, and perhaps one day in the blood. “We should also think about screening campaigns in populations at risk,” suggests the specialist. “But imaging is not very effective in detecting a tumor early on in this deep and difficult to reach organ.” Another avenue, it appears that certain people with pancreatic cancer initially present with glucose intolerance or type 2 diabetes. Monitoring the fluctuation of blood sugar in these patients when they also present unexplained weight loss would make it possible to detect more disease quickly.
Few treatments available
A rapid and sneaky evolution, difficulties in diagnosing it and… a lack of effective therapeutic arsenal, which completes the dark picture of pancreatic cancer.
“In 80% of patients, the tumor is no longer operable at the time of diagnosis,” notes Dr Thibaud Kössler, head of the Digestive Tumors Unit at the HUG Oncology Department. It is possible to offer chemotherapy, which mainly helps to limit symptoms and slow progression, but only rarely offers a cure. Immunotherapy, a therapeutic revolution in recent years which has proven effective for other types of cancers, has proven to be ineffective for pancreatic tumors. “On the research side, work is focused on targeting specific mutations that could complement current treatments,” explains the expert. Personalized vaccines are also being studied.”
While waiting for promising results to lead to effective treatments, patients can benefit from a comprehensive and multidisciplinary care program. “When the diagnosis is announced, we systematically offer support combining nutrition and physical activity, as well as psychological support,” emphasizes Dr. Kössler. Such personalized monitoring brings a benefit to the quality of life, after the shock that the announcement of the illness often represents.
Pancreatitis, another disease of the pancreas
Acute pancreatitis is a common disease, which causes sudden and violent pain in the abdominal area, nausea and vomiting, fever, drops in blood pressure, etc. Alcohol consumption, certain medications, a genetic predisposition or still an immune deficiency can be the cause. It is often linked to the presence of gallstones which obstruct the pancreatic duct and block secretions, causing local inflammation. Repeated acute pancreatitis can eventually cause progressive destruction of the pancreas and lead to what is called chronic pancreatitis. Suffering from this pathology puts you at increased risk of developing pancreatic cancer.
______
Published in Le Matin Dimanche on 11/17/2024
[1] Source: Swiss Cancer League.
[2] https://www.revmed.ch/revue-medicale-suisse/2024/revue-medicale-suisse-884/cancer-du-pancreas-une-epidemie-oncologique-en-devenir
[3] BMI = weight (kg)/height (cm)2