EARLY TAVR Study – According to the presentation by Philippe Généreux and the publication in the “New England Journal of Medicine”.
Key messages
- Early TAVI for patients with asymptomatic severe aortic stenosis has significant advantages over clinical surveillance, including a reduction in unplanned cardiovascular hospitalizations.
- This study revealed that early TAVI, compared to active surveillance, improves short-term clinical outcomes in asymptomatic patients, with a 2-year follow-up.
- Among patients under clinical surveillance, a large proportion (87%) ultimately required valve replacement, highlighting the rapid progression of symptoms in these patients.
Introduction
Current recommendations for the management of asymptomatic aortic stenosis call for regular clinical monitoring. However, with emerging data supporting early surgery in similar cases, the EARLY TAVR study is exploring the impact of an early TAVI strategy in these patients.
Study design
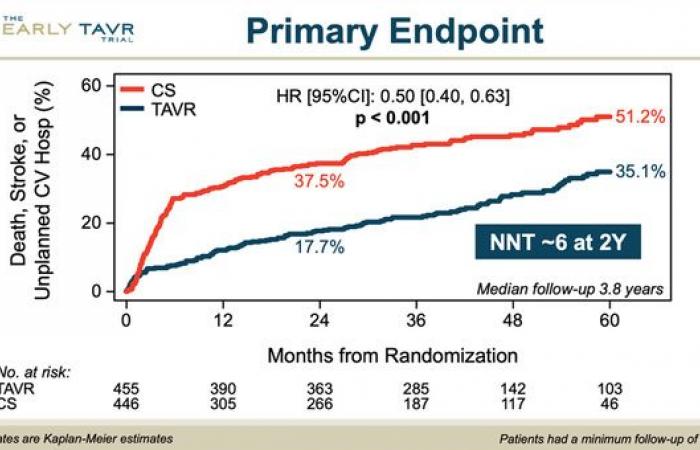
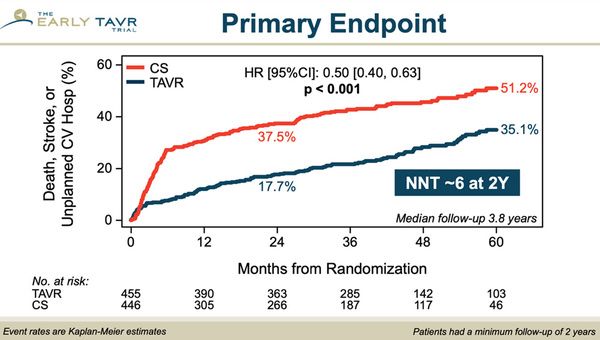
The EARLY TAVR study is a multicenter, randomized study with 901 patients with asymptomatic severe aortic stenosis, comparing early TAVR (SAPIEN 3) to a clinical monitoring strategy. Patients were followed for a composite event of death, stroke, or unplanned hospitalization. Median follow-up lasted 3.8 years.
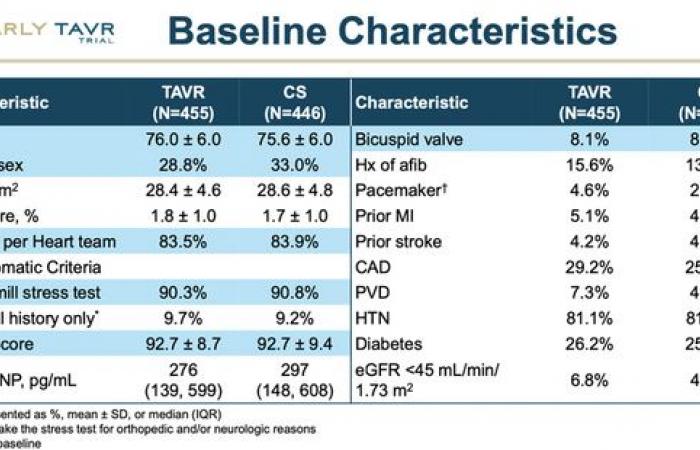
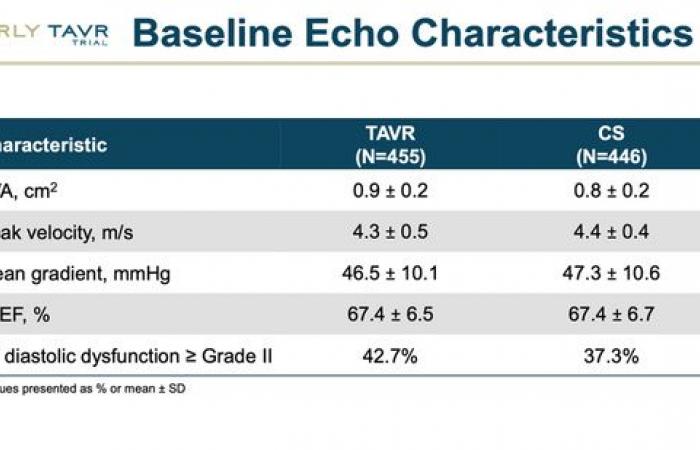
Tableaux 1 : baseline patient characteristics
Results
- Primary event: Early TAVI halved the risk of major cardiovascular events (26.8% for TAVI versus 45.3% for clinical monitoring).
- Primary event components:
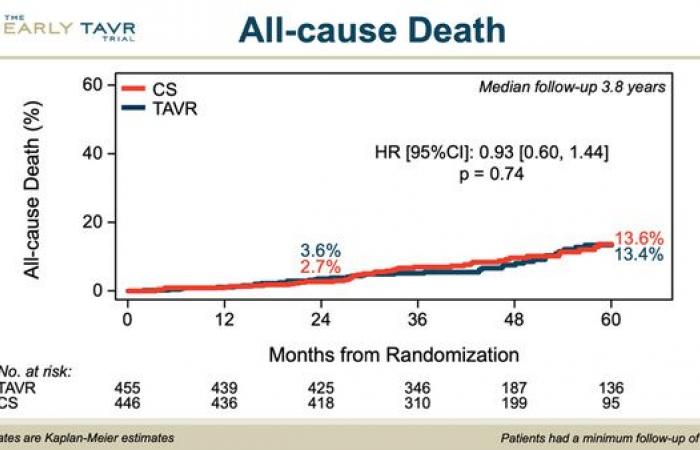
- Death: 8.4% for TAVI vs. 9.2% for surveillance
- Stroke: 4.2% for TAVI vs. 6.7% for surveillance
- Unplanned cardiovascular hospitalizations: 20.9% for TAVI vs. 41.7% for surveillance

Tableaux 2 : study judgment criteria
Conclusion
In patients with asymptomatic severe aortic stenosis, early TAVI significantly reduces serious cardiovascular events compared to clinical monitoring. These results reinforce the idea that early TAVR could prevent rapid deterioration of cardiac function and could influence future management recommendations.
Comments after leaving the room
- The EARLY TAVR study fills an important gap by demonstrating the superiority of an early intervention strategy with TAVI for patients with asymptomatic severe aortic stenosis.
- To properly interpret the lessons of the study, it should be clarified that the clinical monitoring group should not be considered as a “medical” arm but rather as a deferred intervention, because almost 90% of patients ultimately received a replacement. valve during the study. Moreover, 105 of the 388 patients under clinical surveillance underwent an intervention within six months following randomization.
- This study clarifies the natural evolution of severe asymptomatic aortic stenosis, showing that after reaching the echocardiographic criteria for severity, symptoms appear within a relatively short time (6 to 12 months). This highlights the importance of adequate monitoring, discussions with patients and their families about therapeutic strategies and early diagnostic work to prepare for intervention should symptoms appear.
- The trial showed that approximately 40% of converted patients had advanced or acute symptoms (pulmonary edema, class III/IV heart failure, syncope, or cardiac arrest) at the time of surgery. This observation is crucial because it demonstrates the risk of rapid and unpredictable progression of severe asymptomatic stenosis.
- The impact of this study on future recommendations remains debated. The absence of difference in all-cause mortality at 4 years, however, reassures that current practices are up to date.
- To conclude we could quote the author of this work, Philippe Généreux: “there would seem to be no disadvantage to early intervention, especially in light of the natural history of asymptomatic severe aortic stenosis”.
References
Transcatheter Aortic-Valve Replacement for Asymptomatic Severe Aortic Stenosis, NEJM, October 28, 2024
All the news from TCT
Health