According to data from the Bio-Libra register presented at HRS by Valentina Kutyifa.
Key messages
- women with non -ischemic CMP implanted with a primary prevention DAI present a significantly lower rhythmic risk than mensuggesting a potential role of sex in risk stratification.
- Patients with CRT-D have an appropriate event rate (mortality or therapy) than those with a simple DAI.
- Despite the recommendations, the drug treatment remains a real life in real lifeemphasizing the importance of therapeutic optimization parallel to the implantation of the DAI.
Introduction
The implantable automatic defibrillator (DAI) has demonstrated a benefit in terms of mortality reduction in patients with non -ischemic cardiomyopathy with a left -wing ventricular ejection fraction (FEVG). However, the results of these studies go back almost twenty years, even though the drug treatments for heart failure have experienced major progress in recent years, significantly improving the prognosis of patients.
The study DANISH (Buyer et al., Nejm 2016), the most recent on this subject, has not shown any benefit in terms of overall mortality, although a reduction in the risk of sudden death has been observed there. These studies also have a sub-representation of women, not making it possible to reach the statistical power necessary to analyze the differences related to sex.
The register Bio-libra has been set up in the United States to assess the mortality and the occurrence of rhythmic events in patients with non-ischemic cardiomyopathy established with a DAI, with or without resynchronization therapy (CRT-D). One of the specific objectives of the register was to ensure sufficient female representation, set at a minimum of 40 %.
This study aims to specifically explore the differences according to sex and according to the type of device implanted (DAI versus CRT-D).
Methodology and results
It is an academic, multicenter, prospective and observational study. This study aims to include 1,000 patients over the age of 18, suffering from non-ischemic cardiomyopathy, implanted in primary prevention of an implantable automatic defibrillator (DAI) Biotronik, with or without resynchronization, in 48 centers in the United States. Monitoring is planned over a period of three years.
Patients implanted in secondary prevention, with ischemic heart disease, with advanced heart failure requiring cardiac transplant or short -term circulatory assistance in the year following implantation, as well as those with estimated life expectancy for less than a year or pregnant women, were excluded from the study. The inclusion of patients took place between 2019 and 2021. This study was sponsored by Biotronik.
Patients were followed every six months prospectively, via a mixed remote monitoring system and on -site annual visits for three years.
The main judgment criterion was the occurrence of a combined event associating mortality and appropriate therapy issued by the DAI.
Secondary criteria included the separate analysis of the appropriate therapies and the mortality of any cause, evaluated according to sex and the type of device implanted (simple or CRT-D), as well as sudden mortality and mortality any cause according to these same variables.
THE Tertiary objectives Included the evaluation of drug treatment, ultrasound remodeling, therapies appropriate by shock, inappropriate shocks and complications, according to sex and the type of prosthesis.
In total, 1,000 patients were included, including 48 % women. Just under half of the patients had received a CRT-D (49 % of women vs 42 % of men). The average age was 62 years. Fifty -one percent of patients were in class III of NYHA, with an average FEVG of 30 %. Twelve percent had history of atrial fibrillation (10 % in women versus 15 % in men, p <0.001). The majority of patients were treated with beta-blockers (92 %), IEC/ARNI or Arni (80 %), diuretics (75 %) but anti-aldosterone (39 %) and Gliflozines (6 %) treatments were underused.
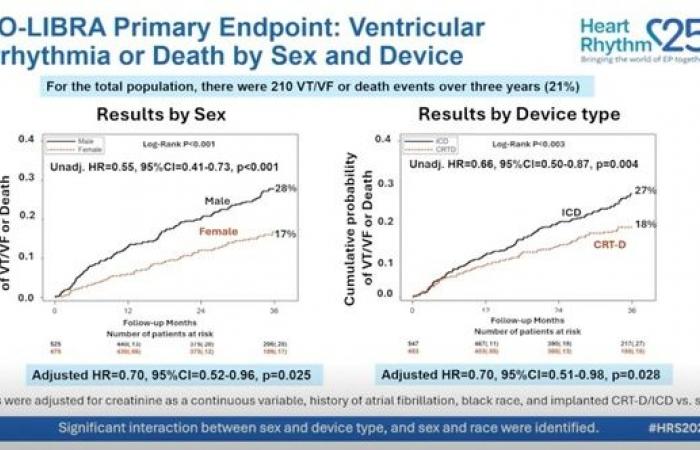
-In the overall population, 210 tachycardia/ventricular fibrillation events (TV/FV) or deaths have been recorded, or 21 % of the cohort. On the criterion of main judgment (TV/FV or death), the event rate was significantly lower in women (17 % versus 28 %, p adjusted = 0.025) and in patients with CRT-D (18 % versus 27 %, p adjusted = 0.028) (Figure 1).
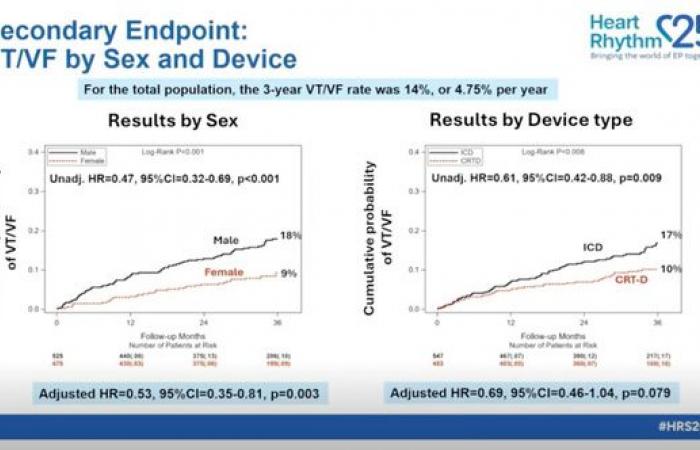
Regarding the TV/FV rate, it was significantly lower in women than in men (9 % versus 18 %, p adjusted = 0.03) (Figure 2). A non-significant trend was observed in patients located with a CRT-D (10 % versus 17 %, p = 0.079).
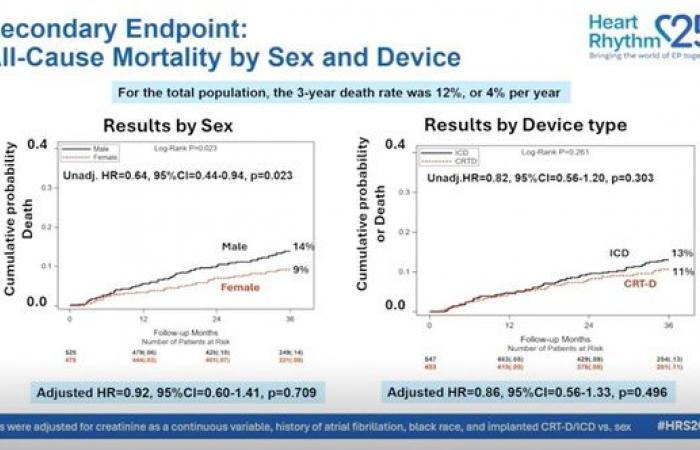
Annual mortality was not statistically different according to sex (9 % in women versus 14 % in humans, p adjusted = 0.7) or depending on the type of device (11 % for CRT versus 13 % for the DAI, p adjusted = 0.49) after adjustment (Figure 3).
The appropriate shock rate at three years was 6.1 %, without difference depending on the sex or the type of prosthesis. On the other hand, the rate of inappropriate shocks, from 10.3 % to three years, was lower in women and in CRT-D carriers.
Conclusion
In conclusion, the data of this prospective register highlight a high rate of events in patients with a DAI implanted in primary prevention in the context of non -ischemic cardiomyopathy. Gender differences have been observed: women present a significantly lower rhythmic event risk than men, suggesting that rhythmic risk could be less in women. This result requires confirmation in other cohorts in order to determine if sex should be integrated, in the future, in the risk stratification algorithms and the indications for implantation of DAI.
In addition, the study highlights a globally sub-optimal drug treatment in this population in real living conditions. The risk stratification strategy in non -ischemic CMPs has evolved considerably in recent years, in particular with the integration of cardiac and genetics. Several randomized trials are expected in the years to come, in particular those guided by imaging or genetic profile, in order to better identify patients at high risk likely to make a real benefit of the DAI.
Finally, other clinical parameters such as age, competitive risk of mortality linked to heart failure or comorbidities must also be taken into account in future therapeutic decision strategies.
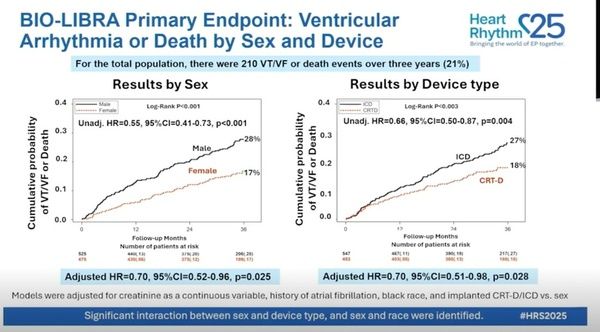
Figure 1
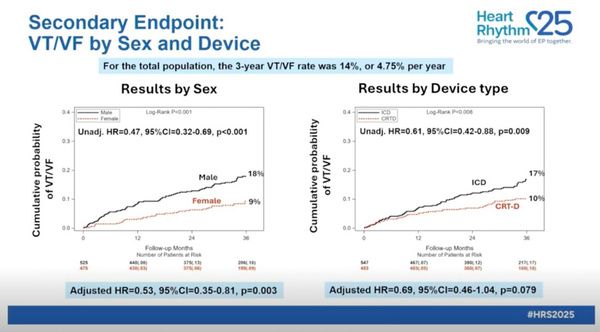
Figure 2
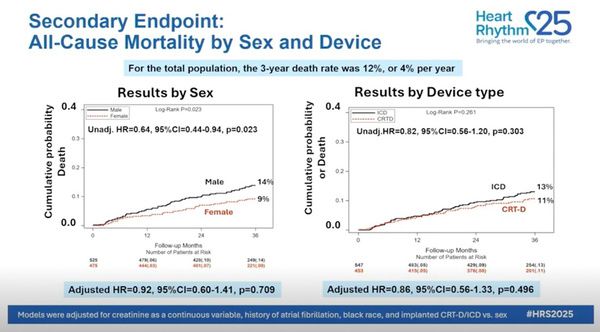
Figure 3
All the news of the HRS 2025
All the news of French rhythm of SFC!