Only four classes of antifungals currently exist and the resistance of pathogens to these drugs complicates treatment.
A research team has identified the fungus’ resistance mutations Candida albicansthe most common cause of fungal infections, for six widely used clinically used drugs belonging to the azole class.
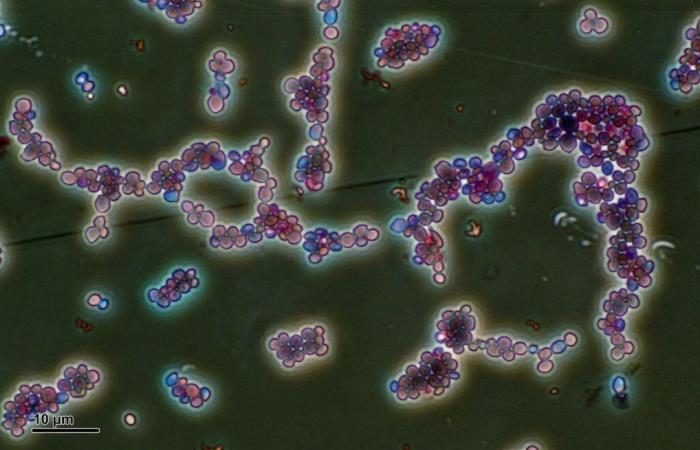
Image Wikimedia
In the study, published in the journal Nature Microbiologythe team grouped the mutations and their resistance to different azoles in a catalog. It can be used by clinical staff to guide them in their choice of treatment.
Camille Bédard, doctoral student at the Faculty of Science and Engineering and first author of the study, highlights the need to find a suitable antifungal quickly, without trial and error.
“The mortality rate can reach 70% for immunocompromised people in the case of the pathogen C. albicans. If clinicians know which mutation they are dealing with, they can look in the catalog to determine the appropriate treatment according to the resistance indicated,” reports Camille Bédard, who works under the direction of Professor Christian Landry.
Worrying cross-resistance
For 88% of resistance mutations, protection is effective for several azole drugs at the same time. As the azoles tested all have the same mechanism of action, the team expected to observe this cross-resistance, but not to this extent. “Azoles act by binding with a protein key to the growth of the pathogen which allows it to be inhibited.
When there is a resistance mutation, the drug can no longer attach to the protein and loses its effectiveness,” explains the doctoral student. As the molecules are a little different from one azole to another, she did not think not that there would be such versatile protection.
The issue of cross-resistance to azoles concerns Camille Bédard, because this family of antifungals is also used in agriculture. “Certain pathogens present in the environment can be found in humans. This is the case ofAspergillus fumigatusa soil fungus whose spores can be inhaled. In an immunocompromised person, it can cause infections.
If the pathogen has already been in contact with an agricultural azole, it could have developed resistance which also protects it from medical azoles,” warns the young researcher, recipient of a 2024 Vanier Scholarship.
In a future article, she wishes to evaluate the rate of cross-resistance between agricultural and medical azoles for A. fumigatus and other mushrooms of the same type.
An exhaustive catalog
Rather than choosing mutations that seem of interest, the team research is interested in all possible mutations, which increases the predictive power of the catalog. “We are able to generate and study mutations which have not yet been observed in nature and which could emerge in the future. Thus, even if a mutation is observed in the clinic for the first time, it will be found in the catalog and the clinician will be able to know whether or not there is resistance,” maintains Camille Bédard. To study the 4000 potential mutations, researchers use a model yeast, baker’s yeast. It is genetically modified to produce the same protein as the pathogen C. albicans which is targeted by the azole drug. They then test resistance by putting all the “mutants” in the presence of each antifungal. Those who survive will be categorized as resistant.
The team now wants to determine whether the resistance mutations identified for C. albicans will be the same in other pathogenic fungi. “Could we use the catalog for other fungi or would we need a catalog for each pathogen?” asks Camille Bédard.
The study was published in the journal Nature Microbiology. The other signatories of theLaval University are Isabelle Gagnon-Arsenault, Jonathan Boisvert, Samuel PlanteAlexandre K. Dubé, Alicia Pageau, Anna Fijarczyk and Christian R Landry. Researchers Jehoshua Sharma, Laetitia Morocco, Rebecca S. Shapiro,University of Guelphalso collaborated.