In total, the AI found 204 cases of breast cancer that would have otherwise been missed by human analysis, the study authors said. It is possible that other cases were missed when the radiologist judged that it was not appropriate to review images flagged by the AI, they add.
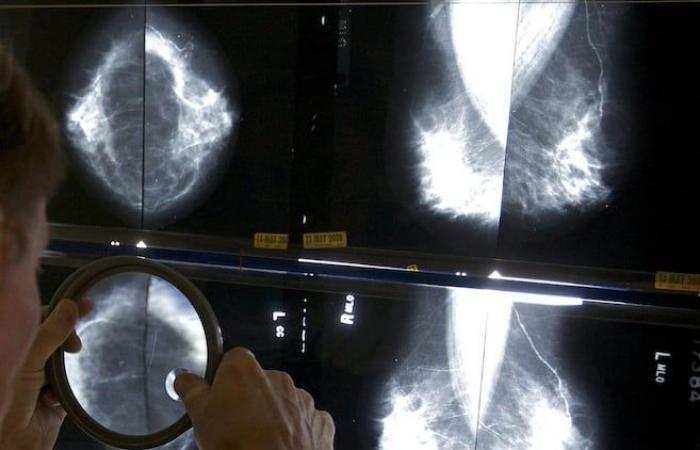
Mammography, commented Dr. Matthew Seidler, head of the breast imaging section at the CHUM radiology department, “is the only screening modality that has been shown to reduce mortality due to breast cancer.”
“But it’s not a perfect exam,” he recalled. The sensitivity of mammography is approximately 87%. And we know that it is a test that is less effective in women who have a high density (…). So there are limits to mammography, hence the idea that the use of AI could increase the performance of this examination not only to find more cancers, but also so that there are fewer false ones. alarms.”
The study involved some 500,000 women who were participating in a breast cancer detection program in Germany. This program provides that all images will be read by two radiologists. If one of them detects an anomaly, the images are sent to a third specialist.
The authors of the study wanted to know what contribution AI could make to this process. Without the help of AI, doctors detected six cases of breast cancer for every thousand patients studied. With AI, seven cases were detected, an increase of 17.6%.
There were also fewer false positive results in the AI group, meaning results that raise suspicion for cancer but eventually turn out to be just a false alarm.
This suggests “that AI could improve cancer detection (…) by detecting cancers detected during the next screening cycle earlier, some of which are visible retrospectively on mammograms from a previous screening cycle,” they said. write the authors of the study in the journal Nature Medicine.
Even if these results are promising, said Dr. Seidler, we must keep in mind that the use of AI to detect breast cancer, particularly at the CHUM where he works, remains “embryonic”. For the moment, the tools in place are mainly used to improve the quality of images.
We also cannot take for granted that the results obtained in Germany would be reproducible in other populations, he stressed, including in Quebec and Canada.
“We sometimes hear that, in the future, certain tasks are going to be done entirely by software,” Dr. Seidler said. But I think that artificial intelligence algorithms will rather help and support the performance of radiologists, to be able to help more patients.”
A lot of effort is also being devoted to developing tools capable of identifying patients most at risk, he added. Certain artificial intelligence algorithms can, for example, predict that a patient, based on the results of her mammogram, has a very high risk of breast cancer over the next five years.
“But for another patient, we are not worried that she will develop breast cancer, so perhaps this patient could be screened every two or three years instead of every year,” concluded Dr. Seidler.