“The problem with neurosurgery,” explains Eelco Hoving, pediatric neurosurgeon, “is that it is unforgiving. » Even specialists often have to first open the patient’s skull to get a better idea of what to treat.
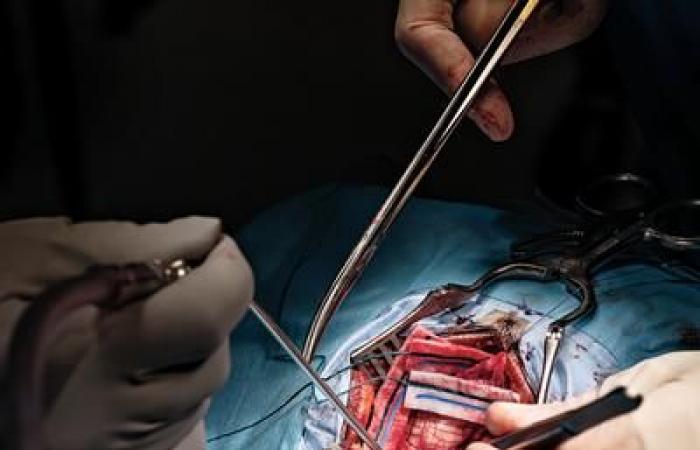
In the case of neurological tumors, for example, doctors often don’t know what they are until they remove a piece of skull and perform a biopsy on a sample of brain tissue. This is the case at Prinses Máxima, a pediatric oncology center affiliated with UMC Utrecht, one of the largest research hospitals in the Netherlands. Eelco Hoving is director of the neuro-oncology department there. The sample is then sent to the laboratory, where it is analyzed in two ways. Pathologists carry out sequencing and profiling of this tissue, and attempt to identify the type of tumor present – a laborious process that can take a week, or often longer. At the same time, the laboratory freezes a small cross-section of the sample and slices it thinly with a scalpel to obtain a sort of “frozen snapshot,” explains Eelco Hoving. This “quick cut” examined under a microscope can help identify the type of tumor in as little as fifteen to twenty minutes, but it is significantly less reliable than the slower method.
Which makes the situation particularly complex for neurosurgeons in the operating room. Which are forced to make a series of delicate trade-offs based on incomplete information: is there actually a tumor? If it is cancerous, is it an aggressive form that needs to be removed quickly? or a milder form that can benefit from less invasive treatment, such as chemotherapy?
Eelco Hoving knows these limits viscerally. He remembers an operation on a young patient a few years ago. The quick cut indicated an extremely malignant embryonal tumor, called atypical teratoid rhabdoid tumor (ATRT). He therefore decided to favor an equally aggressive intervention and opted for radical ablation, removing more than 98% of the tumor tissue. Following the operation, the patient lost part of the motor skills of one of his arms. However, ten days later, the pathology report revealed that the tumor was not ATRT, but something much more benign. “It was a germ cell tumor,” recalls Eelco Hoving, “and it could be treated very effectively with radiotherapy and chemotherapy. » He had made the best decision given the limited information available to him: “I attempted radical ablation with the best of intentions, but, in retrospect, it was not what I should have done. »