Lying on his dad’s lap, Laurent, 5 years old, develops his plans for the future in this touching scene from the documentary film Blinkin theaters from October 4.
Posted at 2:00 a.m.
Updated at 1:00 p.m.
Blinkit’s a film of National Geographic which accompanies the Pelletier Lemay family on their journey around the world, in 2022 and 2023. Edith Lemay and Sébastien Pelletier had a very special mission: to fill the visual memory of their four children.
Three of them – Mia, Colin and Laurent – suffer from retinitis pigmentosa. One of their genes is defective, causing the cells in the retina to gradually die. The disease progresses differently from one person to another (even within the same family), but it leads, for many, to “legal” blindness, and for a small minority, to total blindness. “Maybe I’ll be blind just a little bit…”, hopes Laurent.
On the occasion of the release of Blink and the book Full eyes (signed by Edith Lemay and published by Éditions de l’homme), The Press wanted to talk to scientists who, like Laurent, want to defy fate. “The announcement of the diagnosis is often perceived as a curse, but when we know the origin, we can start working on solutions,” says ophthalmologist José-Alain Sahel, at the heart of this booming research.
Gene therapies
When the Dr Sahel began his practice 40 years ago when the genes involved in retinal diseases were unknown. It was “unbearable” for him, he remembers, to tell patients that he could do nothing about the progression of their illness. Things have evolved since then: 300 genes have been identified, we better understand how retinal diseases develop and how to deal with them. “We can’t promise, because it’s research, but there has never been so much hope,” summarizes Dr.r Sahel.
The therapy that appears the most logical is “gene therapy”; it consists of penetrating a functional copy of the gene into the cell. A first treatment (Luxturna) was approved by Health Canada in 2020. It targets a specific mutation, different from that of Pelletier Lemay.
In Quebec, two children aged 11 and 17 received the treatment in 2023. “In general, the earlier we take children in the course of their illness, the more improvement there is,” explains the Dre Cynthia Qian, who operated on these two children, and who is also the ophthalmologist for the Pelletier Lemay family.
Dozens of clinical trials are underway on other genes. One of them, carried out in France, concerns the mutation in question in the Pelletier Lemays, but the trial is still in its early stages. Among the ongoing studies, some will lead to positive results, but others to mixed or negative results, recalls the Dre Qian.
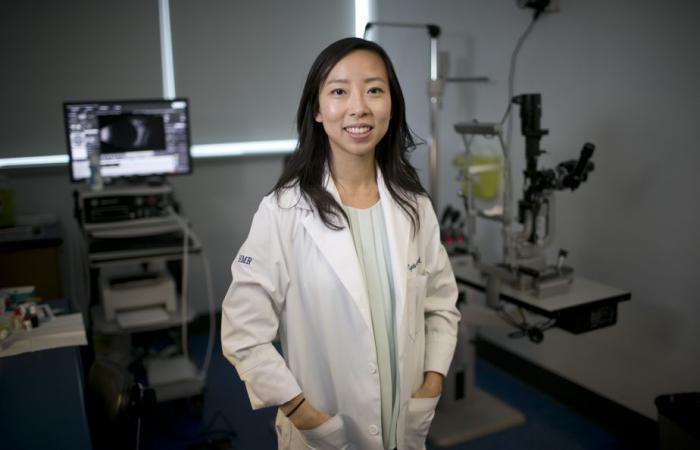
PHOTO DAVID BOILY, LA PRESSE ARCHIVES
Cynthia Qian, ophthalmology surgeon at CHU Sainte-Justine
It is certain that there is a lot of hope, but we do not want to give an unrealistic or too short time frame. When we have expectations, the disappointment is greater.
Dre Cynthia Qian
The sometimes slow progression of the disease complicates clinical trials, notes Dr.r Sahel: “To demonstrate a difference in the progression of the disease, very long clinical trials would have to be carried out, sometimes too long for manufacturers obliged to invest. »
The children’s mother, Edith Lemay, prefers to accept her children’s illness and prepare them to face it rather than clinging to current studies. “Yes, there is hope, but I can’t allow myself to be excited,” she confides. And all this comes with fear, because even if there is a treatment, it will be an experimental treatment. »
Genome editing
Edith Lemay and Sébastien Pelletier recently met another researcher, Dr Fyodor Urnov, professor at the University of California at Berkeley. He has been working for 20 years on a technology called “genome editing”. Here, it is not a question of injecting a gene to replace the one that is lacking, but of to correct the genome language error that causes disease.
The Dr Urnov is also a cinema enthusiast, and by an almost “mystical” coincidence, he was in the theater during the film’s premiere Blinkat the end of August, in Colorado. It was with emotion that he listened to little Laurent dreaming of medicine.

PHOTO TAKEN FROM UC BERKELEY WEBSITE
Fyodor Urnov
“I started crying,” he says, “because such a drug was invented – it’s called CRISPR. »
The Dr Urnov is scientific director of the Innovative Genomics Institute, founded by Jennifer Doudna, a Nobel laureate for her work on a technology with a special name: CRISPR-Cas9. CRISPR systems are often compared to “genetic scissors”: they can identify a precise DNA sequence, cut it and replace it. Quebecer Sylvain Moineau is a pioneer of this technology surrounded by an aura of revolution.
In late 2023, the United States approved the first-ever CRISPR-based drug – Casgevy, which addresses sickle cell anemia, a common genetic disease. Many clinical trials are underway to treat other diseases, including those of the retina.
The current problem is not technical, according to Fyodor Urnov, but “societal”. “Industrialists are interested in diseases that affect a large pool of patients, and that unfortunately does not include Pelletier Lemay children,” he summarizes.
He gives the example of a recent clinical trial that tested CRISPR on a form of retinal disease. Despite “clinically significant results”, the company ended the recruitment of participants in 2022, citing the small pool of potential patients in the United States (300). Create a medicine, recalls the Dr Urnov, it takes four years and 10 to 15 million dollars.
Over the summer, the US Food and Drug Administration published the first guidelines for a “platform” that would make it possible to create personalized treatments more quickly, by taking evidence from already approved drugs and incorporating the same components.
Professor Urnov’s team first wants to organize clinical trials with children suffering from an immune system disease and with less than six months to live. “In the next three, four years, we will learn more and more about the safety and effectiveness of these designer drugs. I think that children with progressive illnesses, like the Pelletier Lemays, should be second in line,” says the professor. Urnov, who wants to emphasize one thing: “no false hope, no false promises”.
For the moment, Mia, Colin and Laurent’s illness is fortunately progressing slowly. They cannot see in dim light, but they still have very good visual fields, so good that they would probably not be eligible for a clinical study, emphasizes Edith Lemay. If the option presents itself one day, “the decision will be made with the doctors, and with the children,” she concludes.
Protect remaining vision
Other parallel approaches are also being studied, including one called “neuroprotection”. The D teamr Sahel is currently leading a clinical trial to test this approach, which aims not to correct the mutation, but to protect the remaining retinal cells, regardless of the gene in question. The Dr Sahel lists other promising approaches: “optogenetic” therapy, which uses the genetic code of an algal protein (!) to wake up retinal cells; the artificial retina; stem cell transplant…