Continuation of our series on research in interventional cardiology presented at the European Society of Cardiology (ESC) congress and reported on the “Practical Cardiology” platform. Tricuspid repair seems very present in current research work, as does the treatment of mitral regurgitation, which is safer if it includes the installation of a dedicated device. There are also questions about coronary revascularization to accompany TAVI.
The “Practical Cardiology” platform presents a review of the various studies presented at the ESC congress held last fall in London. We return here to work concerning structural interventional cardiology.
Tricuspid repair very present in current research work
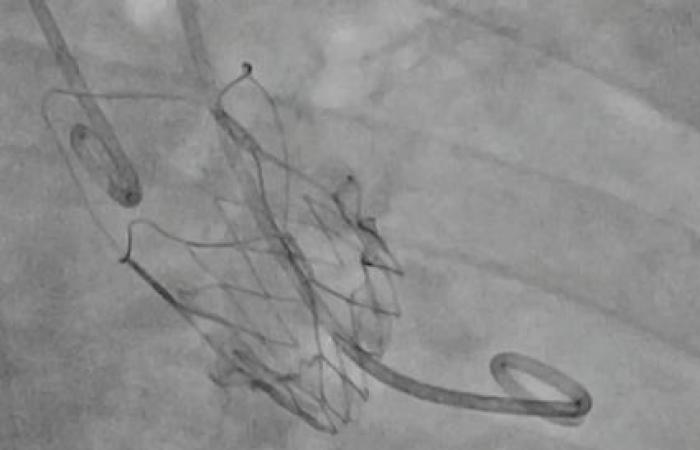
A study on secondary symptomatic severe tricuspid regurgitation (TR) in high-risk patients is first presented. Transcatheter edge-to-edge repair (TEER) and its impact on harsh clinical outcomes such as mortality and hospitalizations remains little explored. Therefore, this TRI.Fr study investigates whether adding TEER to optimal medical therapy (GDMT) could improve clinical outcomes more effectively than GDMT alone in this complex population.
The researchers prove here that it significantly improves clinical outcomes compared to GDMT alone, with a total of 74.1% of patients in the TEER group showing an improvement in the clinical composite score, compared to 40.6% in the TEER group. GDMT group.
TRI.Fr is then compared to TRILUMINATE, which includes a broader range of TR severity, including massive and torrential cases. Results from the TRI.Fr and TRILUMINATE trials support the growing use of TEER as a key treatment for severe TR, especially in inoperable patients. The researchers conclude that adoption of TEER is expected to accelerate with advances in patient screening and procedural technologies.
Treatment of mitral regurgitation is safer if it includes the installation of a dedicated device
The “Practical Cardiology” article then explores the field of heart failure (HF) and moderate to severe functional mitral regurgitation (FMR). The RESHAPE-HF2 trial aims to clarify the impact of percutaneous repair with MitraClipTM, in addition to optimal medical treatment, in reducing the rate of hospitalization for HF and cardiovascular mortality. This work shows that at 24 months, the MitraClipTM group presented superior results to the “control” group, including 37 events per 100 patient-years compared to 58.9 and a hospitalization rate for HF alone of 26.9 events for 100 patient-years compared to 46.6 in the “control” group.
Also worth mentioning is the MATTERHORN trial, which aimed to compare the effectiveness and safety of TEER and surgery in patients with secondary mitral regurgitation.
Questions about coronary revascularization to accompany TAVI
Next comes work falling within the scope of TAVI. A first trial evaluates the impact of coronary revascularization (percutaneous coronary intervention – PCI) in patients with stable coronary artery disease and severe aortic stenosis, candidates for TAVI. Approximately half of patients undergoing TAVR also have coronary artery disease (CAD), of which only 20% will be revascularized. The NOTION-3 trial is exploring the benefit of PCI compared to conservative treatment in these patients candidates for TAVI.
This work shows that PCI associated with TAVR is linked to a reduction in the risk of major adverse cardiac events (MACE), compared to conservative treatment, but that it is accompanied by an increased risk of bleeding. It is therefore important to take into account individual patient characteristics, such as their age, general health, comorbidities and bleeding risk, before deciding whether to perform PCI before or during TAVI.
Still in the field of TAVI, let us cite the POPular PAUSE TAVI trial, which questions the interruption or continuation of anticoagulants during TAVI, as well as the RHEIA trial, which evaluates the superiority of TAVI compared to surgical aortic replacement in women .
Bruno Benque