A few months ago, a team from KULeuven indicated the presence of measles in Brussels wastewater. Which was not really a surprise, given that this highly contagious virus – and dangerous, since it can cause serious complications – is occasionally detected, particularly in Brussels schools. The same for the south of the country, where 88 confirmed cases were recorded as of September 30, 2024 (compared to 15 for the whole of 2023), according to the Agency for Quality Life (AVIQ).
These episodic outbreaks of the disease can be explained by too low a rate of vaccination coverage. “For measles, in 2023 we were at 85% for the first dose and 75% for the second dose”, figures from Vivalis, the Brussels health administration (formerly Cocom). In Wallonia, rates reach similar levels. However, “optimal coverage is a population that is 95% vaccinated”. Furthermore, measles is not the only disease for which collective protection remains insufficient.
Far from the 75% recommended by the WHO
Thus, coverage against the flu does not even reach 50% of people at risk (over 65 years old, patients with chronic illnesses, etc.), in Wallonia or Brussels. Far from the 75% recommended by the World Health Organization (WHO)… In ten years, the situation has barely changed, a study by Mutualités Libres revealed this year. And this, despite awareness campaigns regularly carried out by health authorities. Should this be seen as an effect of the Covid-19 pandemic? In some people, the health crisis has in any case given rise to vaccine hesitancy, which, in others, has completely given way to rejection, transforming them into die-hard “anti-vaxxers”.
“During the pandemic, injunctions have too often been paternalistic and guilt-inducing”
On the other hand, the communication adopted will not always make it possible to change their minds. In a study by the Brussels Studies Institute (BSI), researchers from UCLouvain and ULB pointed out the use, during the crisis, of “paternalistic and guilt-inducing” injunctions. Enough to induce counterproductive effects, by “locking the population into a division between good citizens (…) and bad ones, labeled “anti-vax””, rather than “relieving fears and hesitations”. Certain messages displayed in public spaces (“get vaccinated to reunite with your colleagues”) also seemed out of step with the reality in Brussels.
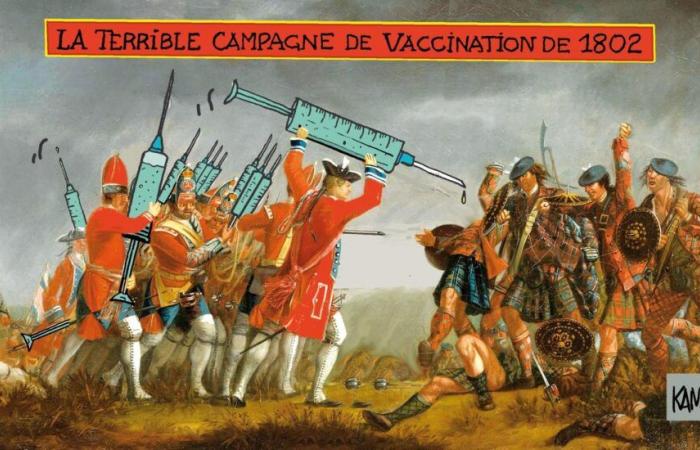
Hide those syringes…
The authors identified other errors: we can question the relevance of messages often accompanied by “images showing syringes”, when the fear of injections affects “up to a quarter of adults”, and that for “16% of adults, this fear leads to refusing or postponing vaccination”.
“In hindsight, certain elements of communication were indeed open to criticism,” admits Nathalie Nöel. This being said, the General Director of Vivalis would like to recall the context of the Covid crisis. “Let us not forget that in Belgium as elsewhere, we were in an emergency situation, of confinement… Today, whether for the flu or for measles, we communicate differently.”
The importance of general practitioners
In Brussels, the Health Administration launched a group vaccination campaign against flu and Covid-19 a few weeks ago. No more displaying syringes. Like last year, awareness messages should emphasize the ease of the process: “Hop! You can get the vaccine at a pharmacy. Get your flu shot. It’s never been so simple.” On the Vivalis side, they say they want to emphasize accessibility to care. “For two years, the procedures have been made easier. There is no longer a need for a prescription. All you have to do is stop by the pharmacy, pick up a dose and go to your doctor. Or to have it injected on the spot; in Brussels, there are around 250 partner pharmacies.” It remains to be seen whether this will prove sufficient. In the BSI study, the researchers recalled the importance of relays of trust, capable of convincing hesitant audiences. General practitioners, as well as religious leaders and associations play a determining role in this regard. The past has shown it: a poorly calibrated message can make certain hesitants lean to the wrong side, although fears or lack of information do not automatically transform them into anti-vaxxers.
Polio in photo
However, the problem is not only communicational. “There are also sociological, cultural, even psychological issues linked to vaccine hesitancy,” says Nathalie Noël. Which, in the case of the most convinced anti-vaxxers, makes the task of getting them to change their opinion very difficult. “The discussions I was able to have with them taught me that it’s wasted effort,” says immunologist Michel Goldman. They have a lot of preconceived ideas, only retain information that goes their way and discard others. Often, parents already have strong ideas, under the influence of the media and social networks.” This is why the ULB professor is trying to raise awareness as early as possible. At their invitation, he regularly visits schools to develop “health literacy, that is to say the acquisition of basic skills to understand and use objective scientific information with a view to taking the right decisions regarding one’s health.”
Not by starting by talking about vaccines, injections and other potential side effects. But rather by recalling the ravages of infectious diseases, such as poliomyelitis. Supporting photos from the last century, “of children equipped with crutches or imprisoned in iron lungs”. Images that do not leave one indifferent, and which then allow the class to embark on the path to this “literacy”. “In my experience, children aged 11, 12 are quite capable of understanding the essential principles of vaccination. Overall, they show unmistakable interest during my interventions.”